Nuclear Medicine
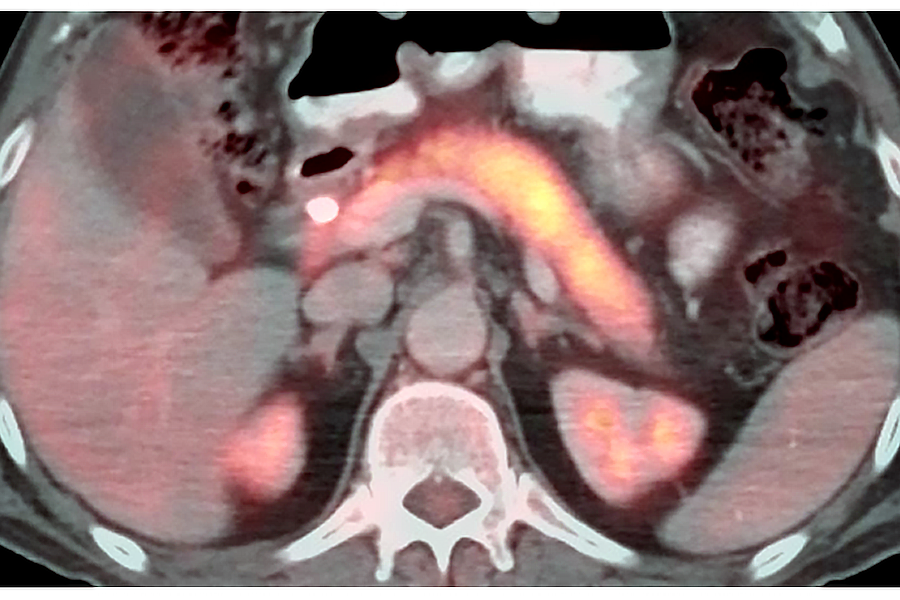
PET/CT imaging uses radiotracers to assess the metabolic or biochemical function of tissues and organs.
The UNMC division of nuclear radiology and molecular imaging is a leader at providing advanced diagnostic nuclear medicine imaging services and therapeutic treatments that are not readily available elsewhere in Nebraska for both adult and pediatric patients. We offer radionuclide diagnostic imaging studies in general nuclear medicine, PET/CT, SPECT/CT, administer radionuclide therapy/theranostics, and perform nuclear cardiology services.
Nuclear radiology can be helpful in providing physicians with both diagnostic and functional physiologic information of the patient’s cells, tissues, or organs. Nuclear radiology helps diagnose and treat a variety of diseases, such as cancer, heart disease and infection. Small amounts of radioactive substances are administered to the patient that serve as radiotracers for production of images which help assess organ function. These unique images can help provide information that often cannot be obtained using other imaging procedures including X-rays, CT scans or MRIs.
Our nuclear medicine expertise and state of the art equipment make us the preferred referral center for many specialty physicians throughout Nebraska and the surrounding region.
We provide an excellent learning environment for our trainees by providing high-quality clinical service to our patients and support our referring clinicians in all aspects of nuclear radiology. The nuclear medicine resident rotation is designed to provide UNMC radiology residents with a core foundation for developing necessary skills to become clinically competent in nuclear radiology after leaving residency.
Didactic curriculum and rotation training provides preparation for certification in diagnostic radiology by the American Board of Radiology and eligibility for authorized user status by the Nuclear Regulatory Commission and/or agreement states. All facets of diagnostic and therapeutic nuclear medicine training are incorporated during this rotation with graduated levels of supervision and responsibility based on level of training. Over time, residents will gain competence in interpretation, protocolling, quality control, and problem solving for nuclear medicine studies including dynamic/static planar imaging, SPECT/CT and PET/CT.
Residents will additionally build knowledge on proper utilization and handling of radiopharmaceuticals, usage of nuclear medicine instruments, and physics behind nuclear medicine imaging equipment. It is not possible for residents to see all of the types of scans or procedures above during their monthly rotation as many nuclear medicine studies may be more rare. Self-directed learning, attending didactic lectures, and reading recommended nuclear medicine textbooks/literature during the rotation will be essential to success. Residents can additionally participate in tumor boards during the rotation including lymphoma, endocrine, sarcoma/melanoma, and head/neck for exposure to nuclear medicine imaging.

Craig Johnson, MD, Nuclear Medicine Division Chief
Dr. Johnson was drawn to radiology because of the field's use of innovative technology to solve complex medical diagnoses. The broad spectrum of anatomic and physiologic processes that can be visualized in radiology and how this contributes to patient management in nearly every other specialty of medicine is fascinating, he said.
What We Do
Our division provides diagnostic imaging of patients with suspected or known illnesses such as malignancy, infection, dementia, intractable seizures, cardiac diseases, or other disorders requiring anatomic/physiologic problem-solving. General nuclear medicine studies include, but are not limited to, the following.
Planar and SPECT/CT imaging
- Hepatobiliary imaging (hepatobiliary iminodiacetic acid scan to assess gallbladder function, biliary leak, pre-y90 shunts, etc.).
- Bone scan imaging (for oncology, bone pain, prosthetic loosening, infection, etc.).
- Gastric emptying (assess gastroparesis with solid meals).
- Renal imaging (assess glomerular filtration rate/function, obstruction, post-transplant, etc.).
- Thyroid imaging (assess for hot/cold nodules, Graves' disease, thyroid cancer, etc.).
- Parathyroid imaging (assess for parathyroid adenomas/hyperplasia, 4D computed tomography and sestamibi fusion technique with contrast).
- Lung imaging (ventilation/perfusion scans, quantitative lung perfusion assessment before thoracic surgery, right to left shunts, etc.).
- Brain imaging (assess brain perfusion in suspected brain death, movement disorders/Parkinson's disease with dopamine transporter scan, etc.).
- Gastrointestinal imaging (assess GI bleed, Meckel's diverticulum, splenic tissue, etc.).
- Lymph node imaging (pre-surgical sentinel lymph node localization).
- Cerebrospinal fluid imaging (neurosurgical shunt function, cerebrospinal fluid leak, cisternography).
- Cardiac imaging (myocardial perfusion rest/stress tests, multigated acquisition scans for ejection fraction, cardiac amyloidosis with pyrophosphate).
- Neuroendocrine tumor imaging (metaiodobenzylguanidine scan in adult/pediatric populations with SPECT/CT).
- Infection/inflammation imaging (tagged white blood cell, prosthesis evaluation, osteomyelitis, etc.).
PET/CT imaging
- F-18 fluorodeoxyglucose for oncology skull to thigh and whole body metabolic imaging.
- F-18 and Ga-68 prostate-specific membrane antigen prostate cancer imaging.
- Ga-68 and Cu-64 dotatate somatostatin receptor positive neuroendocrine cancer imaging.
- F-18 fluorodeoxyglucose for neurodegenerative dementia, seizure, and brain oncology imaging (quantitative analysis).
- F-18 Florbetapir for amyloid plaque/Alzheimer's disease imaging (quantitative analysis).
- F-18 fluorodeoxyglucose myocardial viability and inflammatory/sarcoidosis imaging.
Nuclear medicine treatments/theranostics
- Iodine (I-131) for thyroid cancer and hyperthyroidism (including dosimetry for complex patients).
- Lutetium (Lu-177) dotatate (Lutathera) for advanced neuroendocrine tumors.
- Lutetium (Lu-177) vipivotide tetraxetan (Pluvicto) for advanced prostate cancer.
- Radium (Ra-223) dichloride (Xofigo) for advanced prostate cancer with bone metastases.
- Yttrium (Y-90) radioembolization (TheraSphere/SIR-Spheres) trans-arterial therapy for liver tumors (performed in interventional radiology).