Body Imaging
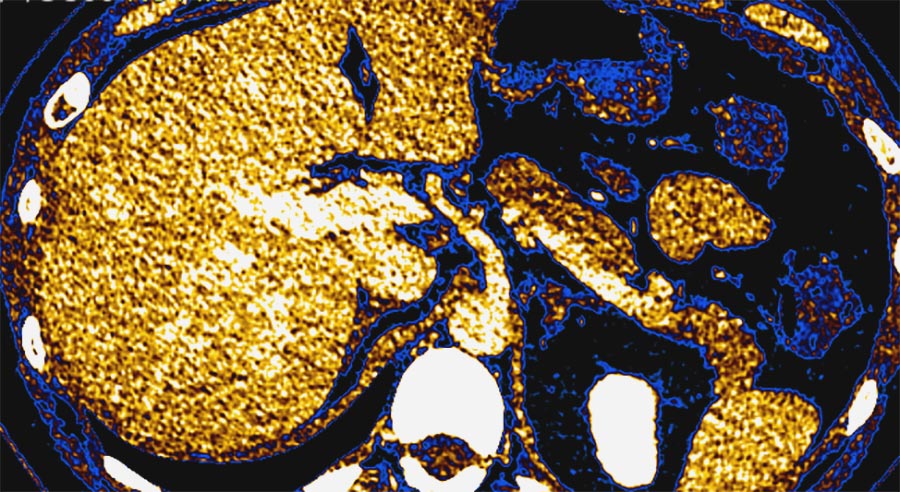
An axial abdominal PET slice.
In the body imaging division, our fellowship-trained dedicated body radiologists provide subspecialty expertise in computed tomography, MRI, fluoroscopy, ultrasound and plain radiographs of the chest, abdomen and pelvis, including benign and malignant diseases and numerous screening exams.
Each of our radiologists is fellowship-trained in this subspecialized field, ensuring expertise and proficiency in interpreting complex images. Furthermore, many members of our division have received additional training and hold expertise in subspecialty areas, such as cardiac, prostate, and virtual colonography imaging.
Our comprehensive services extend beyond routine chest and abdominal imaging and encompass a broad spectrum of imaging exams, such as lung cancer screening, pancreatic imaging, chest and cardiovascular studies, and high-risk liver imaging. We collaborate closely with all medical specialties at our primary clinical partner, Nebraska Medicine, and from outside hospitals, participating in multidisciplinary conferences and research projects to deliver the highest standard of care to our patients.
In addition to clinical excellence, we are committed to education, training, mentorship, research and innovation. With a dedicated residency program in diagnostic radiology and a body imaging fellowship, we actively contribute to shaping the next generation of radiologists.
Contrast enhanced ultrasound
Contrast enhanced ultrasound is an examination utilizing the unique properties of a microbubble contrast agent. This has been a valuable addition to our department’s practice by reducing patient anxiety with a faster time to diagnosis/imaging workup given current wait times for MRIs. The study is ideal for patients with renal failure or insufficiency as the microbubble contrast agent is not excreted by the kidneys, but rather exhaled as a gas by the lungs. Therefore, a multiphasic, contrast enhanced examination for the evaluation of indeterminate hepatic and renal lesions can be performed safely for patients that otherwise might not be able to have an adequate CT scan or MRI.
At our institution, we frequently utilize contrast enhanced ultrasound in the surveillance of non-surgical renal masses, the characterization of cystic renal masses, and workup of indeterminate liver lesions. Contrast ultrasound is an excellent problem solving tool for patients with indeterminate hepatic and renal findings on other imaging modalities or for those patients with inconclusive biopsy results.
GI Fluoroscopy
Gastrointestinal radiology specializes in evaluation of the GI tract using the fluoroscopy machine and enteric contrast material to diagnose anatomic and functional abnormalities. Many exams follow a standard protocol, but others require problem-solving skills to obtain the necessary imaging to answer a clinical question or evaluate for a surgical complication. Different contrast materials are chosen based on the clinical situation and requested imaging. A few genitourinary exams are also performed using fluoroscopy. Resident review of the medical record and any prior imaging is required to determine the best fluoroscopic protocol and contrast to be used.
A radiology resident on this rotation spends each day performing the scheduled outpatient and add-on inpatient exams for each day. Rotation involves learning how to use the fluoroscopy machine and perform all the routine protocols for standard exams such as an upper GI or esophagram. Residents learn through observation first and then supervised hands-on and later independent exam performance. Progressively, residents gain experience with problem-solving type exams that often involve evaluating a patient for post-surgical complications, such as leaks and strictures. After completing a fluoroscopy study, the resident reviews all images with staff and dictates the exam findings. Abdominal radiograph interpretation is also part of this rotation.
Fluoroscopy is a unique modality, as the radiologist and radiology technologists work together to perform the exam, each with distinct responsibilities. Close collaboration with the diagnostic radiology techs is necessary for safe and competent patient care and a rewarding aspect of this rotation.

Jennifer Oliveto, MD, Body Imaging Division Chief
Dr. Oliveto is an award-winning faculty member who has been instrumental in the implementation of new MR protocols for complex disease processes, allowing patients to avoid radiation associated with CT scans.