Fast Facts
As part of our community outreach and education, we provide information and essential facts about Staphylococcus and methicillin-resistant Staphylococcus aureus, commonly known as MRSA, which is a type of staph that has become resistant to penicillin-based antibiotics.
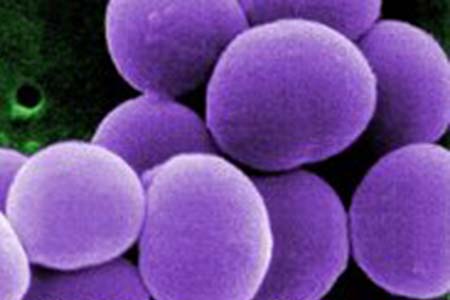
Staph is the common name for a group of bacteria in the genus Staphylococcus, a term that might sound intimidating. By breaking it down, we find that “staph” is Latin for grape-like clusters, and “coccus” is Latin for round, meaning that this is a group of bacteria that appear under the microscope as round, grape-like clusters.
There are more than 30 species of staph, with the most common in humans being Staphylococcus aureus and Staphylococcus epidermidis.
Staph Infection Symptoms
Staph infection can occur nearly anywhere in the body, and can range from a minor infection to a life threatening illness.
Anyone can develop a staph infection, but some groups are at higher risk:
- Newborns.
- Women who are breastfeeding.
- People who frequently are hospitalized.
- Health care workers.
- Intravenous drug users.
- Those with chronic conditions, such as diabetes, cancer, vascular disease and lung disease.
- Those with weakened immune systems.
- Those with skin injuries or disorders, an intravenous catheter or surgical incision or implant.
An increasing prevalence of staph is seen in individuals who play contact sports or live in high density population areas such as military camps, dorms or long-term care facilities.
Diagnosis and Treatment
At any time, an estimated 30% of the healthy human population has staph present on skin or in mucous membranes such as the nose or mouth. Most people have been exposed to staph at one time or another. Usually S. aureus lives on the skin without causing any harm or disease. However, damaged skin, injuries and in-dwelling devices such as implants and catheters can allow the bacteria to overcome the natural immune response of the body and lead to a potentially severe infection.
Skin infections may be treated with topical antibiotic cream and oral antibiotics, depending on the severity of infection. If abscesses are present, they will likely be drained. Serious or life threatening infections are treated with IV antibiotics.
If the bacteria are cultured for diagnosis, the susceptibility of the particular staph strain to various antibiotics will be tested to determine the most effective treatment.
If the infection is associated with an in-dwelling device, such as a catheter or surgical implant, antibiotic treatment alone may not successfully eradicate the bacteria. If this is the case, the in-dwelling device may be removed and replaced.
Prevention
Staph can be transmitted directly, from person-to-person contact, or indirectly by coming into contact with staph on objects such as clothing and sports equipment. Many steps can be taken to reduce one’s risk of contracting a staph infection.
Overuse and misuse of antibiotics have resulted in strains of bacteria, such as MRSA, that require lengthy treatment with new antibiotics or combinations of antibiotics. These new drugs or combinations of drugs are often more expensive and more toxic than older antibiotics. Follow best practices for antibiotic use:
- Use antibiotics for bacterial infections, not viruses such as the common cold.
- Take antibiotics as directed, and finish the entire course.
In some instances, bacteria have become resistant to all available antibiotics – essentially returning us to the pre-antibiotic era of the 1930s, when people routinely succumbed to routine bacterial infections.
MRSA
MRSA stands for methicillin-resistant Staphylococcus aureus, and is pronounced “mursa.”
The overuse of antibiotics over many years has resulted in an ever-growing population of antibiotic resistant bacteria, such as MRSA. Antibiotics are often misused by individuals who take them for viruses, like the common colds. Also, many people who need an antibiotic to overcome a bacterial infection may not take the antibiotics properly, such as not finishing a full course of antibiotics.
Antibiotic-resistant strains of bacteria, such as MRSA,require lengthy treatment with new antibiotics or combinations of antibiotics, which can be more expensive and more toxic than older antibiotics. In some instances, bacteria have become resistant to all available antibiotics