Rural first responders are "hungry" for emergency training. Here's how UNMC's SIM-NE is coming to the rescue.
On long and lonesome highways west (and north and south) of Omaha, emergency medical resources can be few and often, far away.
Small emergency teams are able to customize their SIM-NE training based on their needs.
For rural residents, the individuals helping in an emergency often are neighbors and friends.
“I grew up in small-town Nebraska,” said Paul Paulman, MD, who recently retired as a leader in rural medicine at UNMC. “My hometown had 800 people. I knew the EMS first responders. One ran the filling station, another ran the grocery store.”
Few can match the dedication shown by these community volunteers, Dr. Paulman said. Most have day jobs and devote many nights and weekends a year to mastering an array of life-saving skills. But it can be tough to stay up-to-date with medical technology and procedures and feel well-prepared to handle everything from car crashes to farm accidents to heart attacks, emergency childbirths and more.
Simulation in Motion-Nebraska (SIM-NE) is changing that.
"When you're looking up, I want the person looking down to be the best-trained possible," Dr. Paulman said. "That's what this is all about."
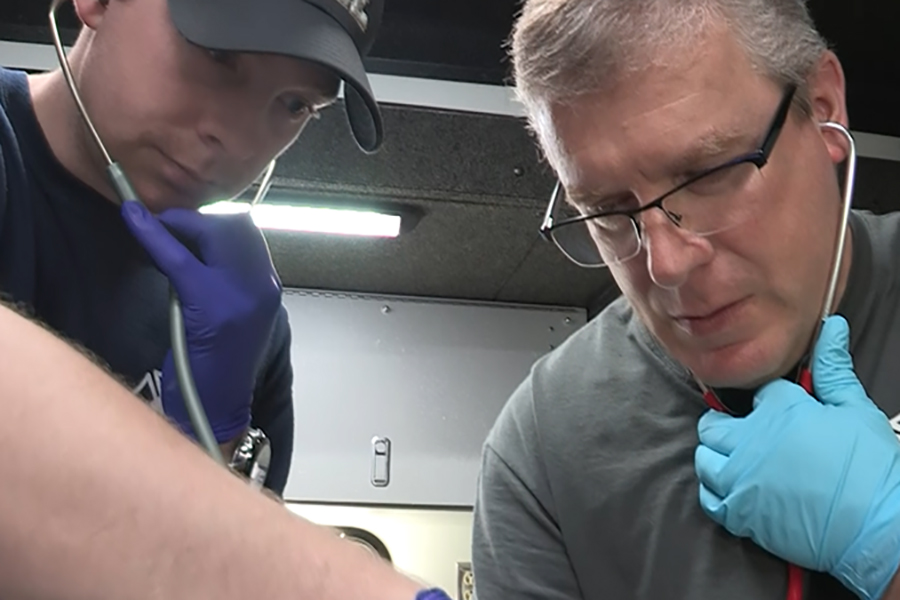
In many small towns, it's neighbors helping neighbors in emergency situations. UNMC's Simulation in Motion-Nebraska takes training to the communities rather than having volunteers travel to larger cities.
SIM-NE, which Dr. Paulman helped introduce, is a statewide, mobile education system that takes state-of-the-art, hands-on training to emergency medical service providers in rural areas across the state, including health professionals in hospitals. SIM-NE provides free or low-cost training via four 44-foot-long trucks customized to replicate real-life emergencies to enhance life-saving skills for those in rural areas.
SIM-NE's fleet, launched in June 2017, is stationed in Scottsbluff, Norfolk, Kearney and Omaha. Rather than have learners in greater Nebraska travel to larger cities, the trainers go to them. This allows training to be team-based as learners train side-by-side with the people they normally work with during an emergency response.

UNMC's Simulation in Motion-Nebraska has a fleet of four customized trucks, each painted royal blue and equipped with high-tech patient simulators, a mobile ER and an ambulance bay.
The training, volunteers say, is invaluable.
"It really makes us stretch our skills that we already have. That way we can provide better patient care to the entire town and Custer County," said Kacey Woodliff, emergency medical technician with Broken Bow Ambulance Service.
“We also train on team dynamics. We train on interprofessional activities,” said Doug Dekker, UNMC’s SIM-NE program manager.
“At 3 o’clock in the morning, in Lynch, Nebraska (for example), there may only be two or three people working. So when that bad patient comes in from the ambulance, it’s the ambulance crew and the nurses on duty working on that person until they can get more help coming in there. So they’ve got to work as a team. And they may not often get an opportunity to do that, outside of those emergencies.”
"They (SIM-NE) tested our abilities, and they made the scenarios real," says Wilber Fire and Rescue Chief Craig Vhynalek.
Each mobile unit is equipped with medical supplies, pre-programmed computerized medical and trauma scenarios, patient simulators, vital sign monitors, heart monitors and defibrillators, audio and video recording/playback capabilities and mock drugs.
Emergency medical volunteers aren’t the only ones to benefit. SIM-NE provides training to critical-access hospitals and professionals who otherwise might need to search far and wide for this type of hands-on practice.
“We started doing some training with school emergency response teams,” Dekker said.
In 2019 SIM-NE took part in FBI SWAT training for agents from across the country by conducting high fidelity simulation scenarios as part of a large final skills testing event.
"The SIM-NE scenarios were both trauma-related and enhanced the skills of the agents in taking care of fellow agents who may be injured during FBI SWAT activities," Dekker said.
SIM-NE also has trained law enforcement on the use of AEDs (automated external defibrillators).
The team is looking into working with long-term care facility personnel, too.
Papillion-LaVista school nurse Annette Jeans said continuing education in her job is critical.
"School nurses are not just band-aids and boo-boos and ice packs. It's real-world care for students and young adults. Instead of us having to go outside to look for the education, it (SIM-NE) came to us."
The “experiential” scenarios allow providers to take test runs at tough or unusual cases — like a complicated emergency birth.
"We know many of our critical care hospitals are doing 50 to 100 deliveries a year," said Ann Anderson Berry, MD, PhD, associate professor of pediatrics at UNMC and interim division chief of neonatology at Nebraska Medicine. "So, a nurse or provider might only see an infant that needs advanced resuscitation or a mom with complications once every three, five or seven years. And taking their medical training and neonatal courses every two years probably doesn't keep their skill set up to where they'd like it to be for high-risk, low-volume deliveries."

Lifelike manikins can be programmed to give EMS providers experience in treating heart attacks and hundreds of other life-threatening conditions. The training, through UNMC's Simulation in Motion-Nebraska, is team-based and free or low cost to small departments and hospitals statewide.
In a holiday movie-miracle coincidence, SIM-NE training saved the day Nov. 14 on a country road near Hildreth.
The town's fire and rescue squad delivered a baby in the back of the ambulance – less than 48 hours after specialized, high-tech training on emergency obstetrics from SIM-NE.
The child, a boy, arrived "Monday, 8:51 a.m., mile marker 32," said proud father Kevin Gregory, of Franklin.
"My jaw is still on the floor when I think about it," said Hildreth Fire and Rescue EMT Elizabeth Burki, who helped deliver the baby. "It makes me teary-eyed."
It’s not a scenario rural EMTs see every day. Or for decades.
"Thank God for the training," Burki said, "I’m not even going to kid you."
Ryan Knaus, who "caught" Raiden as he was being born, called SIM-NE simulation "spot on."
"Everything I did (while training), I did in the back of that ambulance," he said.
Gregory and mom Jasmine Gutschow were headed from Franklin to her doctor in Kearney with two soon-to-be big siblings in the car, when their vehicle broke down. They were almost a month before her due date. But, while the car refused to move, the contractions accelerated.
"I said, ‘You’ve just got to call 911,’" Gutschow said. "We’re not making it."
By coincidence, the father of Jasmine's pediatrician was on the squad, and he got his son, the doctor, on the phone. "Having that connection there really helped," Knaus said.
Burki and Knaus had practiced together, "And that’s exactly how it played out," she said. "He caught that baby, and his attention went to the cord and my attention went to Raiden."
She administered suction and oxygen – just as they’d practiced during their SIM-NE training.
"I am incredibly grateful for it," Burki said.


At left, Hildreth Fire & Rescue volunteers prepare for their first-ever delivery of a baby in the ambulance as the expectant mother's young daughter looks on. At right, Gregory and Jasmine Gutschow with Raiden. The newborn arrived Nov 14, a month ahead of Jasmine's due date.
“It doesn’t happen very often,” Dekker said. “But, when it does happen, by gosh, you better know what you’re doing. This allows people to have a better feel for what that is.”
And that means, when you are the patient looking up, the emergency responder looking down at you is ready to roll.
SIM-NE reaches volunteer first responders in all corners of Nebraska. Director Doug Dekker explains how.
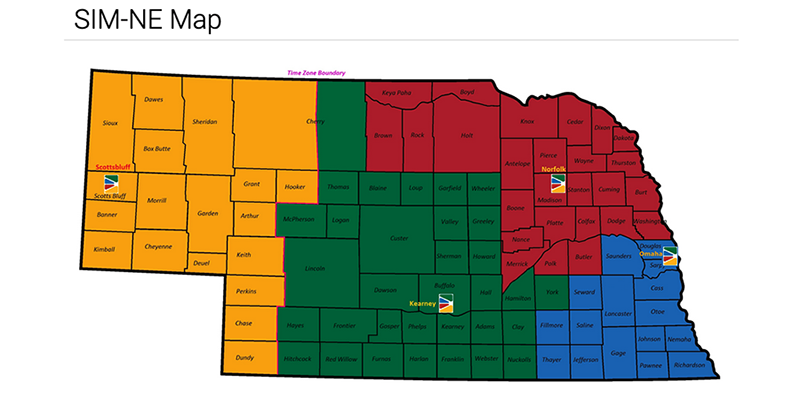
SIM-NE's trucks are stationed in Scottsbluff, Norfolk, Kearney and Omaha in a program that impacts almost everyone in the state, says Director Doug Dekker. SIM-NE is part of UNMC's iEXCEL initiative to revolutionize health care education and training. The goal is to improve quality and safety and reduce costs of patient care through simulation technology. The program was established in large part by a grant from The Leona M. and Harry B. Helmsley Charitable Trust. SIM-NE continues to be funded by private philanthropy.



