Nebraska’s Long Term Care Facilities (LTCF) faced with positive COVID-19 test results of a staff member(s) or resident(s) are receiving infection prevention and control (IPC) guidance from the Infection Control Assessment and Promotion (ICAP) program, the National Emerging Special Pathogens Training and Education Center (NETEC) grant, some of whose leaders also support the Global Center for Health Security (GCHS). By utilizing the strengths of each partnering organization in a collaborative approach, ICAP, NETEC, and the GCHS—in partnership with local Department of Health and Human Services (DHHS)—are helping the state’s LTCFs overcome infection prevention and control gaps and challenges in order to improve the safety of their residents, staff, and community.
ICAP—a UNMC/Nebraska Medicine-based healthcare initiative funded by Nebraska DHHS—provides health care facilities with the results of the latest research and best practices in IPC. Focused on building IPC infrastructure in Nebraska, ICAP offers no-cost, peer-to-peer infection control assessments and recommendations as well as ongoing education, updates, and mitigation strategies. The program also provides mentorship opportunities for new infection preventionists (IP) and various tools and resources to assist with quality improvement. During the current pandemic, ICAP team members have been on call 24/7 to coach and guide LTCF in COVID-19 prevention and mitigation strategies. They have developed a remote coaching model for LTCF experiencing COVID-19 outbreaks. Remote coaching models pair an IP from the LTCF to a subject matter expert at ICAP who then remains in contact with the IP and continues to provide guidance until the outbreak is overerts at ICAP.who provides l that pairs an IP from the LTCF to an experienced IP s ttools andNF are starting to r. In addition, ICAP provide real time updates in a weekly webinar for this stakeholder group.
NETEC is a collaboration between faculty/staff from Emory University, Bellevue Hospital Center, New York Health and Hospitals Corporation, and the University of Nebraska Medical Center/Nebraska Medicine and is funded by the Assistant Secretary for Preparedness and Response and the Center for Disease Control and Prevention. NETEC’s mission is "to increase the capability of United States’ public health and health care systems to safely and effectively manage individuals with suspected and confirmed special pathogens." NETEC’s website provides COVID-19 educational materials, training resources, webinars, and online courses.
The GCHS is the nation’s primary biosecurity resource—home to the federally-funded National Quarantine Unit and the leader in primary infectious diseases training programs. With a mission to advance and innovate health system preparedness and response in highly hazardous communicable disease(s), the GCHS embraces a comprehensive, collaborative approach with ICAP and NETEC.
Reports, to date, from Nebraska DHHS, Nebraska Electronic Disease Surveillance System and ICAP indicate:
- 496 LTCFs in Nebraska
- 223 facilities (44%) have been affected by COVID-19
- 70 facilities have received a COVID-19 onsite visit
- 920 LTFC residents have tested COVID-19 positive
- 837 LTCF staff have tested COVID-19 positive
- 178 LTCF residents have died
While Nebraska’s fatalities have remained comparably low to other states, IPC vigilance is key to reduce the transmission of the virus—especially as positive test results continue to occur at Nebraska LTCFs. ICAP serves on the frontline of IPC. When notified a facility has a COVID-19 positive resident or staff member, ICAP assesses the situation with the facility, assists in problem solving any immediate issues of concern, and provides remote coaching.
ICAP uses 1:1 remote coaching to guide contact tracing, identify an isolation strategy, inform about resident and staff cohorting, and facilitate a testing strategy to find additional cases based on potential exposure. In addition, ICAP offers weekly education (specific to long term care) via their popular and interactive webinars, and they house a variety of templates and tools on the ICAP website. Dr. Muhammad Salman Ashraf, Nebraska ICAP Medical Director, explained, "LTCF leadership, IP, and frontline staff are working very hard to keep COVID-19 out of their facilities. However, when it enters their building, it can be very challenging to prevent further transmission. Knowing they have 24/7 access to ICAP subject matter experts is usually a morale booster for everyone at the facility." He then added, "They know they can ask us anything, and we are there to help them in any way we can."
When appropriate, ICAP encourages a facility site visit to provide additional IPC guidance. A team from NETEC, many of who are leaders of the GCHS, schedules a site visit with the facility to help discover and mitigate risks. These visits are non-regulatory in nature. The onsite visit’s purpose is to understand the facility’s current response to COVID-19, share information, provide technical assistance, suggest enhancements in review of workflows or cohorting strategies, review cleaning practices, provide hands on personal protective equipment (PPE) training, and answer any questions.
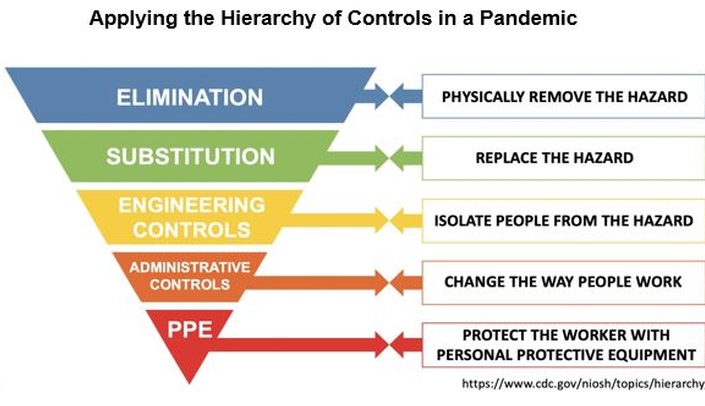
Site visits begin with a survey/interview between the onsite visit team members and the facility’s leadership to discuss workflow, highlight concerns, and complete a quick review of facility demographics, processes, procedures, and protocols. "There is nothing more powerful than walking into a facility, having a conversation with the leaders, and walking through the facility using the hierarchy of controls framework and our checklist, seeing the workflows and staff wearing their PPE" explains Shelly Schwedhelm, Executive Director of GCHS. The hierarchy of controls (see above) is a framework used to mitigate risks; the controls are listed in order of most effective to least effective.
The most effective control is elimination and next is substitution. However, physical removal of the virus would require a COVID-19 vaccine—until we have a vaccine, this control as well as substituting something else for the virus cannot be implemented. Engineering controls are designed to remove the hazard at the source. High efficiency air filters and installation of physical barriers are examples of engineering controls that physically isolate people from the hazard. Administrative controls will change the way people work in order to mitigate the hazard. Workflows, physical distancing, enhanced cleaning/disinfecting strategies are some of the ways to minimize the risk of transmission as well as conserve personal protective equipment (PPE). The least effective form of control is PPE because it is subject to human error—it can be worn incorrectly which negates its effectiveness, and it may malfunction. Despite its level of effectiveness in the framework, PPE is still a critical intervention to protect the worker. There is no single intervention that will alone make the difference, but implementing several of these strategies will reduce risk of virus transmission.
By comparing the facilities’ operation against the hierarchy of controls while touring facilities, the team can discover situations or processes that require mitigation and provide advice on strategies to mitigate the risk. Shelly Schwedhelm emphasizes while education and coaching via virtual technical assistance is a vital component of a multi-faceted approach, site visits are integral to the process, "I think it’s hard to fully comprehend what a facility needs until you see it up close and in person. I’ve seen staff in respirators that are too small for their face, doors to rooms with COVID positive residents open, and fans in use. These situations are much more easily discovered when visually seen and followed up with prompt technical assistance onsite."
Unfortunately, a common issue found is improper healthcare worker masking techniques. Webinars on donning and doffing are provided to facilities via ICAP webinars, but the on-site team also takes the time to meet with staff to provide mask and PPE education. Each type of PPE has varying nuances with its use, and the team provides guidance regarding the specific type of PPE being used at the facility. By not only explaining but also physically demonstrating proper donning and doffing techniques, the team is able to help the facility’s staff overcome knowledge gaps regarding PPE.
Other common concerns include proper zoning of patients and staff, workflow logistics, and the proper use of cleaning supplies. Cohorting staff and patients together in the same "zone" makes it easier to contain the spread of the virus if a person tests positive. Logistics such as meal delivery to residents are examined and suggestions are made if safer alternatives are available. The onsite team also visits with housekeeping to ensure they know the contact time of a disinfectant (the length of time the product requires in order to properly disinfect) and it meets the facility’s needs. By physically visiting the facility, these issues are more easily discovered and corrected with guidance provided to the facility’s staff or leadership.
With so many staff and residents at risk across the state, "Our team of experts will keep working hard to help these facilities," Shelly Schwedhelm said, "and we must look towards the future to determine how healthcare leaders can leverage improved support for infection prevention and control interventions and enhanced education and training to reduce the impact of these types of situations in long term care for the future."