UNMC researchers will study a promising new approach that targets the nerves controlling heart function, potentially transforming the way chronic heart disease is treated.
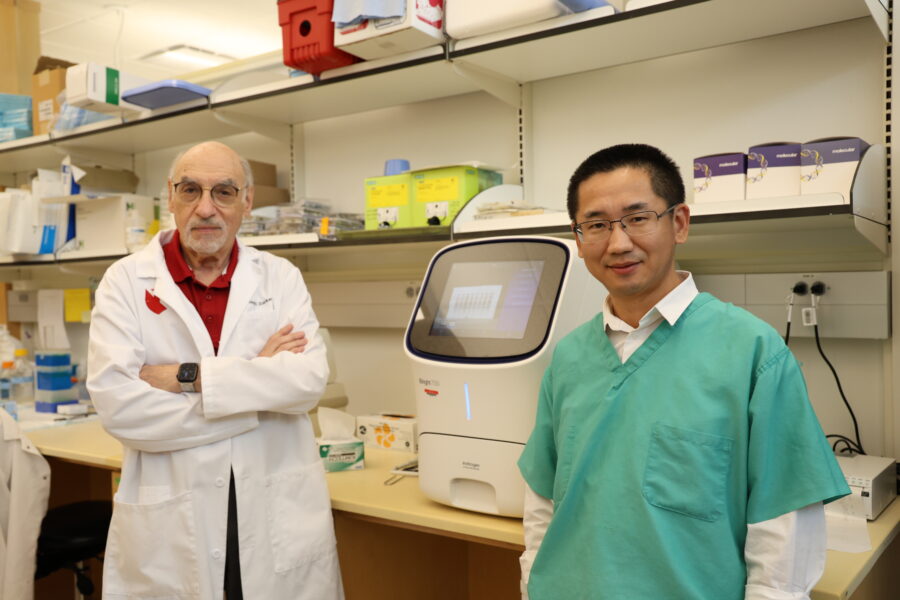
Hanjun Wang, MD, a cardiopulmonary researcher in the UNMC Department of Anesthesiology, and Irving H. Zucker, PhD, in the Department of Cellular and Integrative Physiology, received a $3 million National Institutes of Health grant to conduct the study. They are investigating the role of oxidative stress and inflammation within the nervous system, focusing on a key protein known as NRF2. Their findings could offer a new therapeutic path for treating chronic heart failure.
Dr. Zucker, the Theodore F. Hubbard Professor of Cardiovascular Research in the UNMC Department of Cellular and Integrative Physiology, said the duo’s research journey began over a decade ago when they became interested in the role of oxidative stress in various diseases.
Oxidative stress, a condition where reactive oxygen molecules damage cells, has long been implicated in a range of health problems, from cardiovascular disease to cancer.
“We knew that oxidative stress could affect nerve cells and disrupt their function,” Dr. Zucker said. “We began exploring how to balance oxidative stress with antioxidants and discovered that NRF2 plays a crucial role.”
NRF2, a protein responsible for regulating the body’s antioxidant response, turned out to be more than just a regulator of oxidation — it also plays a significant role in reducing inflammation, Dr. Zucker said.
In heart disease, particularly in cases of chronic heart failure following a heart attack, the nerves that control heart rate and contraction become inflamed, contributing to arrhythmias. This led the team to hypothesize that manipulating NRF2 could help reduce inflammation in these nerves, potentially offering a novel treatment for rhythm disorders.
Dr. Wang, the Margaret R. Larson Professor of Anesthesiology said one of the challenges in treating heart disease involves the stellate ganglion, a collection of nerves that regulates the heart’s rhythm. Current treatments involve anesthetic blocks or surgical removal of the stellate ganglion, a highly invasive procedure. While the anesthetic approach is effective for a short time, repeated injections are necessary and surgical removal only is performed in a few specialized centers due to the complexity and associated risks, he said.
Drs. Wang and Zucker seek to find a less invasive, long-lasting solution. “What we’re proposing is to deliver a localized therapy using NRF2 activators that calm the nerves and reduce inflammation without the need for permanent nerve removal,” Dr. Wang said.
By leveraging new drug delivery systems, they will utilize a gel formulation that allows for the localized, sustained release of NRF2 activators. The goal is to inject this gel directly into the stellate ganglion, suppressing the abnormal nerve activity that leads to arrhythmias, while minimizing side effects.
Interestingly, some of the NRF2 activators used in the study are derived from compounds found in everyday foods, such as curcumin from turmeric and sulforaphane from broccoli. Dr. Zucker said these substances have been used in other areas of medicine but applying them to cardiovascular disease is a newer concept.
“Although these substances are widely available as dietary supplements, the amounts found in food are too small to be effective in therapeutic settings,” Dr. Zucker said. “Our research involves concentrating these compounds to deliver a potent dose directly to the affected nerves, offering a targeted solution.”
Dr. Wang attributes the success of the research to the collaborative nature and interdisciplinary approach. Dr. Wang, mentored by Dr. Zucker for nearly two decades, also partnered with Bin Duan, PhD, an investigator in UNMC’s Mark and Dick Holland Regenerative Medicine Program. Dr. Duan’s expertise in biofabrication was crucial in developing the localized drug delivery system.
“This interdisciplinary approach, combining expertise in physiology, anesthesiology and cardiology, underscores the importance of collaboration in medical innovation,” Dr. Wang said.
“We’ve shown that when departments work together, we can push the boundaries of what’s possible,” Dr. Zucker said. “This collaboration has opened the door to more translational research that can directly impact patient care.”
Mohanad Shukry, MD, PhD, interim chair of the department, said collaboration, including mentor-mentee relationships, is very important for a successful career in research and medicine. “UNMC is fortunate to have such a great example of a successful collaboration,” Dr. Shukry said. “Their work is inspiring, and this new grant validates yet again their outstanding efforts.”
While the research is still in its early stages, its potential to revolutionize the treatment of heart disease is promising. Drs. Wang and Zucker said next steps involve moving from animal models to clinical trials, a process that could take several years but is bolstered by the fact that many of the materials used are already FDA-approved.
“Our ultimate goal is to develop a therapy that can be used widely and safely, providing a long-term solution for patients who currently have few options,” Dr. Wang said.
“With his initial steps at UNMC under Dr. Zucker’s tutelage, Dr. Wang’s tremendous ingenuity, tenacity, and humility have now made him one of the leading scientists in his field worldwide,” said Karsten Bartels, MD, PhD, the department’s vice chair of research. “The fruitful results of the longstanding scientific collaboration between Drs. Zucker and Wang represent a case in point on how successful mentoring relationships vertically advance science. I am humbled to call them my colleagues.”