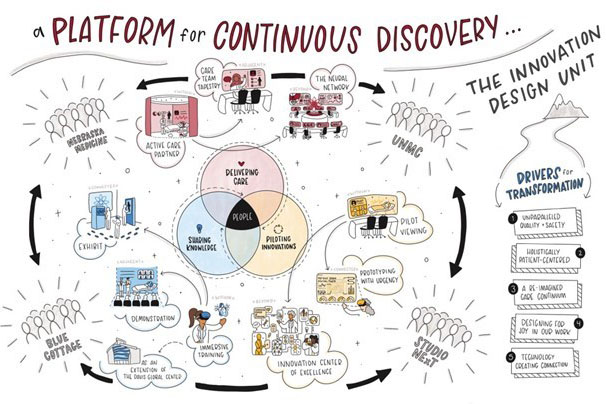
The word “innovation” often is heard when it comes to the ever-changing landscape of health care. Innovation can be a driving force in aiming to transform lives to create a healthy future for all individuals and communities.
One of the ways Nebraska Medicine is steering the implementation of innovation efforts is through an Innovation Operating Model workstream that engages colleagues throughout the health system. The IOM was developed during the conceptualization phase of the Innovation Design Unit.
Putting the Innovation Operating Model in motion
“We know that innovation is an important aspect of Nebraska Medicine, but we also know that because the concept of innovation can be so broad it can also pose challenges,” said Calli Sibilia, Innovation Design Unit project manager.
Sibilia adds that one of the tasks posed to a group led by Breanna Hetland, PhD, and Bethany Lowndes, PhD, and consisting of clinical nurse specialists, physicians, research operations, operational improvement, clinical informatics, nursing professional practice, analytics, and various ancillary teams, was to create a connected, efficient and equitable system of innovation across the organization.
“We also wanted to create the structure and cultivate relationships that would allow the IDU to be a constant point of view on the future of care delivery and transformation,” she said.
This is where the creation of the IOM comes in to help foster these efforts. The above-mentioned group of Nebraska Medicine and UNMC colleagues was tasked with 12 objectives to achieve during a two-year span leading to the opening of the IDU.
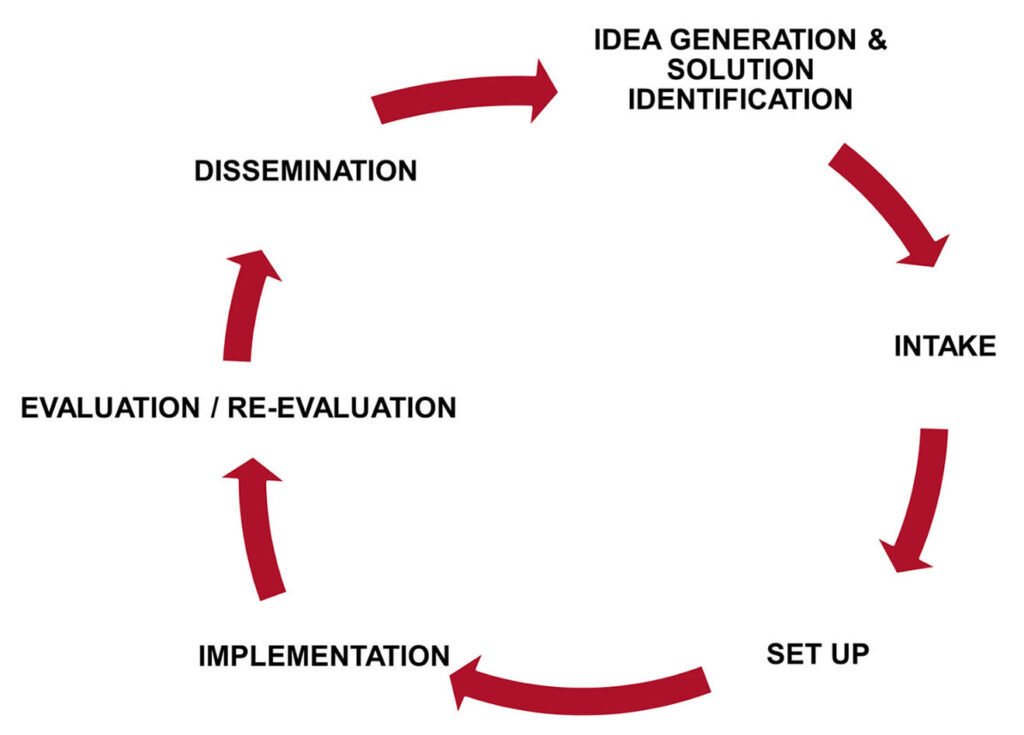
The group’s process started by understanding innovation in its current state at Nebraska Medicine so it could then establish a standard, equitable, closed-loop innovation intake and implementation process. The group designed the process to include components based on the Agile Implementation Framework and the published work “Agile Implementation: A Model for Implementing Evidence-Based Healthcare Solutions into Real-World Practice to Achieve Sustainable Success” by M. Boustani, J. Azar and C.A. Solid, in partnership with the workstream and various internal stakeholders.
The graphic below outlines the innovation cycle that will be adopted in the IDU.
What the Innovative Operating Model means for the future
“The goal of this process, and the all-encompassing innovation program that will live within the IDU, is to establish and evolve the program allowing anyone, regardless of role or department, to submit innovative ideas for consideration in the IDU,” Dr. Lowndes said.
Submitted projects will go through a rigorous evaluation to determine intake based on IDU target criteria. Selected projects will then be supported in the IDU through setup, implementation, evaluation/re-evaluation and dissemination.
“As the IDU innovation program is launched, we will phase the intake process to ensure timeliness as we establish capacity for review,” Dr. Lowndes said. “Meanwhile, the IDU innovation program will include many options for engagement.”
The first phase of this strategic growth consists of two objectives:
- Engaging the design team working on Project Health, the first phase of Project NExT, to work with clinicians in solving the design needs of the future.
- Soliciting solutions from across the health system to address a problem or challenge identified by the enterprise. (The specific problem is yet to be determined.)
Through the bridge space, a design and testing area adjacent to the IDU, the IDU team will invite clinicians and community members to engage in innovation. This will allow for opportunities to learn about and provide feedback on the projects, new technologies and initiatives through the IDU.
Work is underway to ensure data is available for colleagues to plan future projects. This is especially exciting for new technologies previously not available at Nebraska Medicine, such as the RTLS system.
“It’s critical the IOM be built around transparency and equity,” Dr. Hetland said. “Transparency fosters trust and accountability, while equity ensures that advancements benefit everyone, reflecting our commitment to inclusive care. Together, these principles create a robust foundation for sustainable innovation and excellence in health care delivery.”
Being Agile with the Innovation Program
Sibilia said that the IOM will be supported by a thoughtfully designed governance structure, constructed in a way intended to support the unit’s agile nature while ensuring alignment with organizational initiatives, priorities and strategy. This includes an internal and external advisory board and a robust innovation appraisal committee.
“As with all innovative things, we know this is just a starting point for us,” Sibilia said. “We fully acknowledge and expect to learn from every success and failure we encounter and will apply our own agile model to the growth and maintenance of this program.”
Kudos to this team and for inviting an innovation and growth mindset to your important work! Onward and upward!