UNMC has long been at the forefront of research and development of ultra-long acting antiviral therapy (ART) designed as vaccine mimetics for pre-exposure prophylaxis (medicine taken to prevent HIV), extended viral suppression and to facilitate in the elimination of HIV-1 infection. Now, the UNMC scientific team has extended their know-how by developing libraries of ultra-long acting medicines.
This effort has taken a major step forward with the publication of new data today. The data shows that a daily, effective oral treatment used by patients living with HIV worldwide can be, in animal models, transformed into a single, annual injectable.
Clinical trials may start as early as 2023, researchers said.
Physiochemical and pharmacokinetic (PK) formulation properties of an integrase strand transfer inhibitor (INSTI) prodrug nanocrystal facilitates slow drug release. The identified macrophage storage "depot" at the muscle injection site permits drug dissemination through the body at sites where the virus replicates throughout the year.
These research findings for the INSTI prodrug were published today in Nature Communications in an article titled "Transformation of dolutegravir from daily oral to ultra-long-acting parenteral injectable."
"It is the ultra-long extended duration of action of this new investigative UNMC prodrug (XVIR-120) that is the game-changer," said Benson Edagwa, PhD, associate professor in the UNMC Department of Pharmacology and Experimental Neuroscience (PEN), who designed the prodrugs and formulations. "Currently, daily regimen adherence to oral antivirals effectively suppresses and prevents HIV — if you don’t forget to take your pills."
But anyone who has had to stick to even a temporary 10-day prescription knows how easy it is to miss a day.
"Poor adherence to treatment is one of the major impediments to improving the quality of care around the world, whether it is the treatment for chronic illnesses or the prevention of infection," said Paul Domanico, PhD, senior director of global health sciences at the Clinton Health Access Initiative. "The University of Nebraska Medical Center team stands out as a catalyst for introducing novel products to address this head-on. Specifically, the future for antiviral therapy rests in long-acting medicines."
Trading daily pills for a single, annual shot addresses not just forgetfulness and access to re-fills but also, for many, the stigma of taking anti-HIV medication.
Primary investigator Howard Gendelman, MD, Larson Professor of Internal Medicine and Infectious Diseases at UNMC and a driver for this effort for the past two decades, said turning a trusted, existing antiretroviral drug into a long-acting compound was a substantive UNMC victory.
"Dolutegravir is an important medicine for HIV-1 seropositive patients, with over 17 million people worldwide on daily oral therapy today," said Siddappa Byrareddy, PhD, a professor in the PEN department and study collaborator. "We are looking forward to leveraging this INSTI’s existing safety and validation."
"We are working to swiftly move our own proprietary ultra-long acting prodrug formulations to the clinic," said Dr. Gendelman.
They hope to do so by taking their science from the laboratory to the finish line by partnering with industry — including their own company, Exavir Therapeutics, a spinoff co-founded by Drs. Gendelman, Edagwa, and Alborz Yazi, the company president.
The pharmaceutical industry’s excitement in UNMC’s findings is reflected in its interest in Exavir, Yazdi said. The company recently closed on a $4 million "seed financing" led by AlleyCorp with participation from Gilead Sciences.
If successful, the technology also could become applicable in the fight against hepatitis, tuberculosis and other infectious diseases, and that work is just beginning.
"Nebraska scientists are leading this international effort in creating not one ultra-long-lasting antiviral, but now multiple medicines," Dr. Edagwa said.
The compounds are created on the UNMC campus at the Nebraska Nanomedicine Production Plant.
The UNMC team
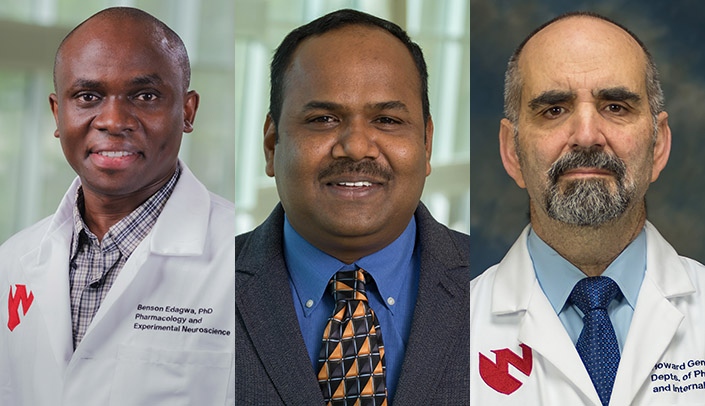
Benson Edagwa, PhD, associate professor of pharmacology and experimental neuroscience, chemist, designed the prodrugs and formulations.
Brady Sillman, PhD, instructor, and Suyash Deodhar, senior graduate student, performed the laboratory and animal experiments, meticulously analyzed the data.
Siddappa Byrareddy, PhD, professor of pharmacology and experimental neuroscience, an expert in host-virus dynamics, drug testing and toxicology.
Sean Avedissian, PharmD, and Anthony Podany, PharmD, assistant and associate professor of pharmacy practice and science, conducted pharmacokinetic simulations.
Howard Gendelman, MD, Larson Professor of Internal Medicine and Infectious Diseases, virologist and immunologist, developed the experimental schemes needed for pharmacological testing and development.