UNMC, in partnership with Nebraska Medicine, has been awarded a $9.5 million grant from the Centers for Disease Control and Prevention (CDC) to enhance infection prevention and control (IPC) initiatives in small and rural health care facilities and advance the ability of health care workers to provide safe and effective clinical care.
Three innovations are being proposed for this project:
- the Isolation System for Treatment and Agile Response for high risk infections (ISTARI) Care Cube 2.0;
- the Mixed Reality for Consultation, Assessment and Education; and
- the NICS Innovation Test Bed Network.
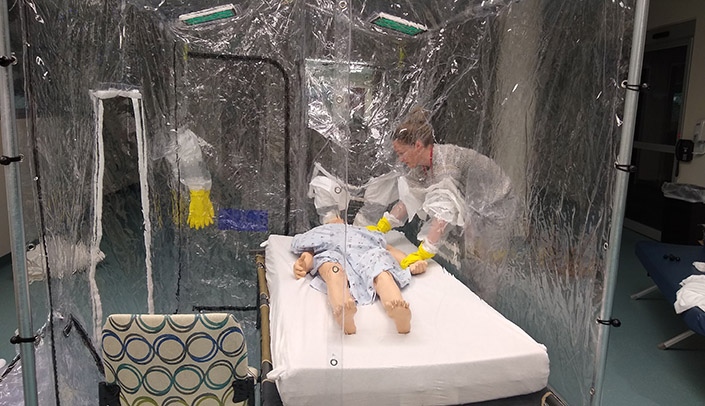
ISTARI Care Cube 2.0
The ISTARI Care Cube 2.0 is an advanced, independent, modular and field-adapted version of ISTARI Care Cube.
“It is intended to enable safe infection prevention and control practices and provide highly effective patient care in the field in a manner that is highly scalable,” said James Lawler, MD, director, international programs and innovation, Global Center for Health Security (GCHS). “ISTARI is a negative pressure envelope that is easily portable and can be assembled in minutes. It features an integrated, HEPA-equivalent air filtration and ventilation system; flexible, transparent walls for patient interactions and procedures; airlock pass-through chambers; and compatibility with routine hospital equipment and facilities.”
By discovering and implementing the paradigm shift of wrapping the PPE around the patient (rather than the health care worker), the ISTARI unit is able to drastically conserve the burn rate of PPE, Dr. Lawler said. In turn, there is less risk to the health care worker and less risk of nosocomial transmission overall. ISTARI 2.0 increases the national capacity for IPC during the COVID-19 pandemic as well as provides for future public health emergencies.
“Many health care settings endure gaps and challenges to IPC programs, and UNMC/Nebraska Medicine intend to resolve these issues with mixed reality for consultation, assessment and education,” Dr. Lawler said.
Mixed Reality for Consultation, Assessment and Education
Mixed reality is an environment where physical reality and digital content are combined to enable interaction with real world and virtual objects — blending real world and digital settings. It is a fusion of technologies that will be used to assist rural and acute facility infection preventionists with training, assessment and mentoring.
“By designing a virtual hospital with various infection prevention and control (IPC) scenarios, local IPs can use the virtual reality environment to frequently train additional staff through engaging technology while maintaining and updating their own skills with more comprehensive hands-on IPC challenges,” said Pam Pizzi, Nebraska Regional Disaster Health Response Ecosystem consultant. “IPs can also engage with virtual subject matter experts using an artificial intelligence ‘chatline’ to find immediate, authoritative answers to pressing issues or, alternatively, complete holistic self-assessments for their facility.
These assessments lead to various resource referrals, including a virtual consultation/mentoring session where local infection preventionists can engage with a remote infection-control expert using 360 cameras and enhanced glasses to identify and rectify IPC concerns for their facility.
The NICS Innovation Test Bed Network
The GCHS will establish a NICS test bed network to ensure the generation, transfer and translation of IPC innovations for varied clinical environments in frontline and critical access facilities. GCHS’s outreach includes more than 32,500 health care workers and 109 facilities of varying size, both domestically and internationally.
“The innovation test bed will allow us to take innovation and put it in places where they will be used for patient care,” said David Brett-Major, MD, professor of epidemiology in the UNMC College of Public Health. “The more we are able to bring innovation into the test beds, the more we can ensure these ideas are developed, and are developed in a way they will be useful.”
By the end of the project period, the program will have identified gaps as well as opportunities to optimize IPC in small, rural health care facilities; increased the ability of small, rural facilities to implement mitigation strategies; and accelerate the development of novel approaches to advance isolation care.
Our Global Center for Health Security team continues to lead the world in practical solutions to real life issues that can be crucial in austere settings. Looking forward to see these all become reality.