Nebraska Medical Center on April 15 began using a new device, called an Infectious Aerosol Capture Mask (IACM), developed by Steven Lisco, M.D., chair of the UNMC Department of Anesthesiology, to capture exhaled aerosolized particles at their source from patients.
 |  |
Steven Lisco, M.D. | Nicholas Markin, M.D. |
Approved by Nebraska Medicine’s Innovation Committee, the hospital is deploying the IACM in the operating room for use with asymptomatic, COVID-unknown patients undergoing monitored anesthesia care, during and following emergence from general endotracheal anesthesia, as well as in the post-anesthesia care units (PACU).
Patients with COVID-19 respiratory illness produce microscopic aerosol particles, which fill a COVID-19 patient’s environment and increase risk of disease transmission. A small percentage of patients also may produce aerosols when asymptomatic or presymptomatic.
Such asymptomatic patients are a challenge for providers, as they may unknowingly produce infectious aerosols when coughing, wearing supplemental oxygen or undergoing aerosol-generating procedures such as intubation and extubation — all common occurrences in operating rooms and the PACU.
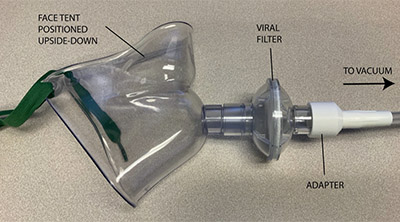 |
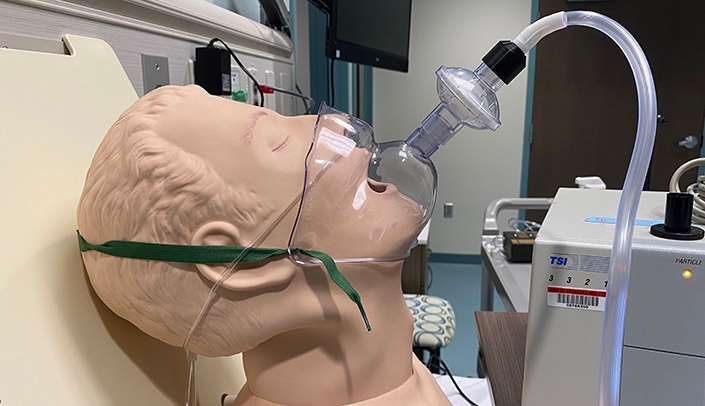
The IACM device developed by Dr. Lisco uses a face tent, positioned upside down with a viral filter attached, connected to wall suction. The apparatus attaches to the vacuum source via standard suction tubing adapted to the device via a plastic piece created with a 3D printer by Nicholas Markin, M.D., director of perioperative imaging.
“The IACM performed very well in laboratory testing when used with a nasal device used to deliver supplemental oxygen, catching more than 90% of airborne particles expelled in the mask, ultimately preventing the aerosol from entering the patient environment,” Dr. Lisco said. “Even when the vacuum wasn’t turned on, the mask was still 85% effective as a barrier.”
“In these areas, patients are often given nasal cannula oxygen, which has been shown to increase the rate and density of aerosolized particles,” Dr. Lisco said. “Additionally, work in these areas often mandates that patients and health care workers be in close proximity. While risk of infection transmission is extremely low, efforts to reduce environmental aerosol contamination are still justified. Using this device with COVID-19-positive patients who require supplemental oxygen also will be beneficial for reducing health care worker risk in the intensive care unit.
“We think it is far superior to put this device on patients in the PACU or ICU versus a surgical mask over a nasal oxygen delivery device,” Dr. Lisco said. “This is a game of inches, and we’re in the red zone. We will do anything we can do protect our health care workers and our community.
“We’re grinding it out a yard or two at a time in classic Husker fashion. This is just another way to shave risk.”
An unintended consequence may be that the device could inadvertently also suction away the oxygen that anesthesiologist is trying to deliver to the patient's lungs through the nasal cannula.
Well done, Drs. Lisco and Markin!
This is so impressive. It only goes to show that during times of crisis, healthcare professionals become more creative and innovative. Your creation is game changing! Congratulations and thank you, Dr Lisco and Dr. Markin (Touchdown!) Lisa Walters
such a great but simple idea. Just like the clear plastic box with side holes for your hands to work through, that goes over the patients head when intubating . Looks like people are stepping up to figure this out. Great and thanks
It is great to see so much innovation during this time. However, I agree with Dr. Lorena Baccaglini that this may have unintended consequences and the device should be tested in a randomized clinical trial, not just in the laboratory environment.
Such an awesome innovation Drs. Lisco and Markin !!
Impressive innovation at our Nebraska Medical Center!👍
Thank you everyone for the positive comments. Happy to answer questions. Thought I would address the issue with respect to potential hypoxia that has been raised. Here are my thoughts:
I do not think it is possible to cause hypoxia with this low level vacuum in an open system as the pressure gradient is not high enough and the mask is not sealed on the face. When wearing the mask you do feel the entrainment of air around the mask. But since it is room air (RA), you cannot dilute RA with RA, nor selectively remove oxygen from the environment utilizing a vacuum. That said, we do agree that one of the possible consequence of use in select patients is that the increased entrainment of room air that might dilute out oxygen levels administered using a nasal cannula by possibly diluting the nasopharyngeal reservoir that is established during routine cannula use. To date we have not found this to occur but If this were to occur it should be easily overcome by adding additional low flow oxygen. We expect the converse to also be true, meaning that if no suction is applied and the mask is used purely as a barrier (still 85% effective by our estimates), it would act as an oxygen reservoir (on a non rebreather FM reducing RA entrainment) and could actually increase saturations. My advice is to use a pulse oximeter when using the mask, as we always would in the OR and PACU.
Hope this helps and thank you for the excellent questions.
Great innovation!