A graduate student from the University of Nebraska Medical Center was the lead author of a study which found that restoring blood flow to the legs of patients with peripheral artery disease (PAD) may stop the progression of scarring in their leg muscles.
Results of the preliminary research were presented on May 5 at the American Heart Association's Arteriosclerosis, Thrombosis and Vascular Biology/Peripheral Vascular Disease 2016 Scientific Sessions in Nashville, Tenn.
PAD causes pain and fatigue while walking due to poor blood circulation in arteries that supply blood to the limbs. The decreased blood flow can lead to substantial scarring and damage in leg muscles.
There are currently no available treatments once the scarring has occurred. Supervised exercise therapy and revascularization procedures (which reopen or bypass blockages in the blood vessels) may help PAD patients walk further and longer, but it is not known if these treatments affect the scarring process.
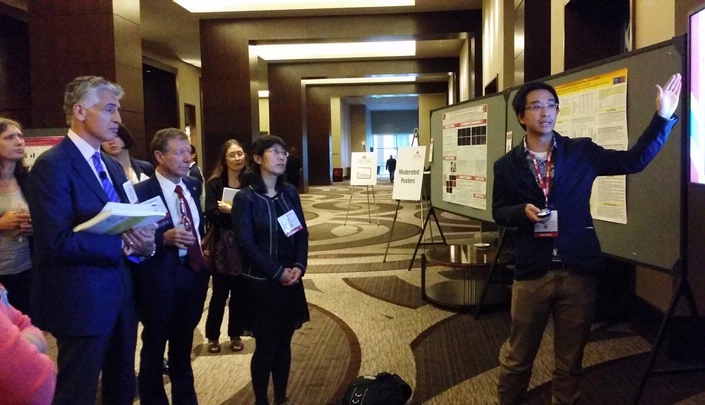
Duy Ha, a doctoral candidate in cellular and integrative physiology, was the lead author on the study. Ha, who is pursuing a combined M.D., Ph.D. degree, was one of only six researchers who were selected to give a moderated poster presentation in which he gave an oral presentation on the poster in front of a crowd of researchers.
Co-authors on the study from UNMC included George Casale, Ph.D., associate professor, surgery-general surgery, and Iraklis Pipinos, M.D.; professor, surgery-general surgery.
The study is funded by the National Heart Lung and Blood Institute, National Institute of Aging, and the Charles and Mary Heider Fund for Excellence in Vascular Surgery. The VA Nebraska and Western Iowa Health Care System provided additional support.
Researchers looked at levels of transforming growth factor-beta (TGF-β1), a protein that promotes scarring, and the amount of collagen (tough protein fibers found in scars) in calf muscle biopsies from patients with PAD severe enough to be considered for surgery.
Six months later, they compared changes in biopsy results among 30 patients who underwent revascularization, 25 who participated in a supervised exercise program, and 17 who had no treatment.
Among the findings:
- Scarring factors – collagen fibers and TGF-β1 – increased in the exercise and control groups, but not in the revascularization group;
- Patients in both the revascularization and exercise groups increased their maximum walking time on treadmill, before calf pain made it impossible to continue;
- Only patients in the revascularization group improved the distance they could walk in six minutes.
- Neither exercise nor revascularization treatment reversed scarring that had already taken place in the calf muscles.
"Increasing blood flow to the leg with revascularization procedures halted the progression of scarring and allowed the patients to walk longer and further," Ha said. "This suggests that the long-term benefits to the health of leg muscles is better with revascularization than with exercise therapy alone. Unfortunately, not all patients are candidates for these procedures, which carry significant risks, and the treated vessels may get blocked again.
"We hope that we can develop therapies that directly decrease TGF-β1 and its associated scarring in the leg muscles of PAD patients. Such new treatments, when used alone or along with revascularization and exercise, may maintain or enhance the ability of our patients to walk and live healthy lives."
Ha won travel awards from the Society for Vascular Surgery and the Atherosclerosis Thrombosis and Vascular Biology Council of the American Heart Association to allow him to share this work at the conference.
"Duy Ha has been an outstanding and highly productive graduate student," said Irving Zucker, Ph.D., professor and chair of the UNMC Department of Cellular and Integrative Physiology. "His research was a blend of clinical and basic science and shows the value of clinical and basic science departments co-mentoring graduate students."
We are Nebraska Medicine and UNMC. Our mission is to lead the world in transforming lives to create a healthy future for all individuals and communities through premier educational programs, innovative research and extraordinary patient care.
Twitter | Facebook | Instagram | YouTube | Flickr