In today’s orthopaedic landscape, getting a total hip or knee replacement no longer has to mean several days in the hospital followed by weeks of recovery.
For many patients at UNMC and our hospital partner, Nebraska Medicine, a quick recovery from a joint replacement is slowly becoming the norm – and the UNMC adult reconstructive surgery team plans to keep it that way.
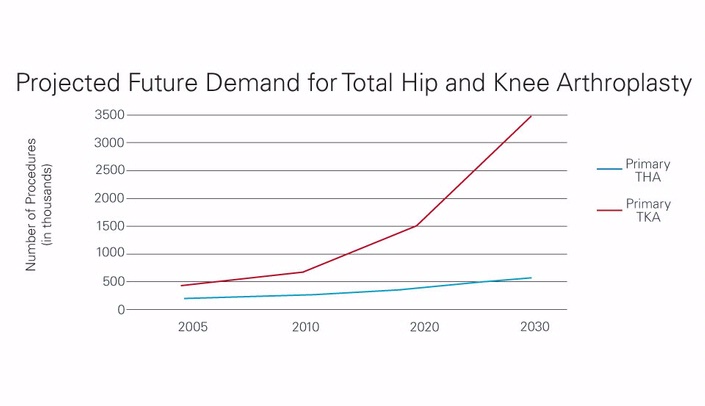
A 2007 study led by Steven Kurtz, Ph.D., projected that by the year 2030, the number of patients seeking total hip arthroplasties will increase 174 percent. Similarly, total knee arthroplasties are expected to increase more than 600 percent.
Pair this with the 2015 expansion of the Hospital Readmissions Reduction Program to include THA and TKA, and orthopaedic surgeons have a unique challenge in front of them.
The question: How do you cater to higher patient volumes while also keeping hospital readmission rates down?
The answer: Establish a fast-track recovery regimen.
In November 2014, Drs. Kevin Garvin, Beau Konigsberg and Curtis Hartman did just that. The three orthopaedic joint surgeons started a Rapid Recovery Program for patients undergoing total hip and knee arthroplasties and have carefully tracked their results since.
"The program is aimed at reducing the length of stay for THA and TKA patients," Dr. Garvin said. "We are always trying to improve our care by decreasing complications and getting patients out of the hospital and back home or to work sooner."
The program relies on a coordinated effort between the joint surgeons, anesthesiologists, physician assistants, nurses, Preop/PACU and OR teams and physical/occupational therapists. Pre and post-surgery patient education is a key factor in decreasing hospital length of stay, as is reducing the amount of pain medication and providing earlier interaction with physical and occupational therapists to reduce immobility.
Over the last few months, the team has seen gradual positive results. Hospital stays have decreased from approximately four to two days in younger, healthier people and from nine to four days in older patients.
In addition, the percentage of people discharged to a skilled nursing or rehabilitation facility has dropped dramatically. Since December 2014, more than half of knee replacement patients and almost 75 percent of hip replacement patients are instead sent home for recovery. The ultimate goal is to send everyone home for recovery, eventually reducing or eliminating the need for skilled rehabilitation care.
"Patients who benefit from the Rapid Recovery Program experience less pain, a reduction or elimination of narcotics after surgery, are able to recover function more rapidly, can return to work sooner and see a cost savings as a result of less time in the hospital," Dr. Garvin said. "These benefits are not only available to younger patients; it has also been shown that patients over age 85 see the most difference in length of stay and readmission rates."
While reducing length of stay is a main priority of the Rapid Recovery Program, it is important to note that the team was able to maintain patient satisfaction and readmission rates.
Another goal of the program was to discontinue the use of Foley catheters in TKA and THA patients to enable earlier mobility. This drastically reduced the number of catheter days in the inpatient unit; as a result, there have been no cases of catheter-associated urinary tract infections since November 2014.