Researchers at UNMC have received a five-year, $3.5 million grant funded by the National Institutes of Health to find out why stents don’t work as well for peripheral arterial disease (PAD) as they do for other arteries outside of the legs.
It’s a big problem – the U.S. Centers for Disease Control and Prevention estimates about 8 million people in the U.S. have PAD, including 12 percent to 20 percent of individuals older than age 60.
Not to mention the problems PAD causes for those who suffer – it reduces or completely cuts off blood flow in the leg arteries which results in pain and numbness of the feet, inability to walk, wounds that won’t heal, and, in worse case scenarios, amputation of the toes, feet or legs. The risk factors include diabetes, smoking, high blood pressure, high cholesterol, obesity and aging.
Jason MacTaggart, M.D., a vascular surgeon, and Alexey Kamenskiy, Ph.D., a biomedical engineer, both assistant professors in the UNMC Department of Surgery, are co-principal investigators of the research study.
“There are several ways to treat PAD and all of them leave significant room for improvement,” Dr. MacTaggart said.
“It’s frustrating for doctors and patients. Everybody is trying to build a better mouse trap, but nobody has. With the support of the surgery department and our team of collaborators, we are taking a rational approach to figuring out why stents don’t work so well in the legs.”
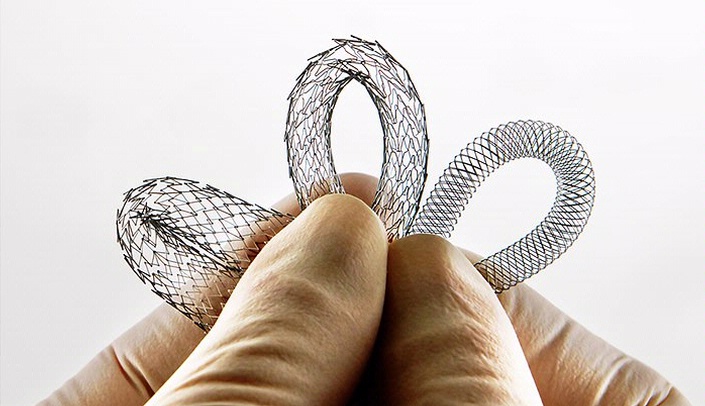
In the past decade, there’s been an explosion of PAD treatment with stents – a less invasive procedure than traditional surgical bypass in which the patient is awake and usually leaves the hospital the next day. Vascular surgeons place stents to help relieve the blockage.
Stents, small tubular metal devices that doctors put in diseased arteries to keep them open, work well in the heart, but often fail miserably in the leg arteries. Stent failure requires almost half of treated PAD patients to have repeat procedures after only one or two years, Dr. MacTaggart said. One national study estimated the cost of PAD treatment at $21 billion a year, much of which is attributed to repeat procedures.
The research team will approach the problem similar to how Boeing designs airplanes or Ford makes cars – with engineering. Using computer models, engineers will work with the medical research team to determine how the artery functions in the leg and then determine how stents work with the artery.
“There’s a lot of work being done in the coronary and carotid arteries but significantly less in the peripheral arteries,” Dr. Kamenskiy said. “The reason why there are so few studies is that leg arteries are difficult to study – the lesions are long, the arteries aren’t as easily accessible and it’s difficult to get donor human tissues to study.”
Researchers will study donor cadavers and arteries of various ages and stages of disease to gain accurate information to design computer models that will be used to determine which stent is best to use in individual patients. The computer predictions will be verified in PAD patients receiving stents at Nebraska Medicine, UNMC’s primary hospital partner, and the Omaha VA Medical Center.
Dr. Kamenskiy said the goal is to improve stents and to personalize PAD interventions.
“We analyze how these stents go into the artery, how they interact with the arterial wall as we walk, and how to make this interaction more favorable,” he said. “Right now there’s a lot of art to using stents in PAD. We are trying to do less art and more science.”
For more information, contact Karen Taylor at UNMC at 402.559.3935 or Holly DeSpiegelaere at the VA, 402.995.4171.
Issue underscores importance of organ, tissue donors
Jason MacTaggart, M.D., a vascular surgeon, and Alexey Kamenskiy, Ph.D., a biomedical engineer, said they are able to approach the problem in a unique way because of those who’ve donated their bodies to science and organ donors who’ve said yes to tissue donation.
“We are grateful to donors and their families and to the Nebraska Organ Recovery System,” Dr. MacTaggart said. “If someone donates their heart or liver, they help one person. If someone donates their arteries to research, they are potentially helping millions of people.
“There is no replacement for human tissues in science. If we don’t have human tissues to study, we’re severely hampered in advancing discoveries in medicine and surgery.”
After your research what where your findings. I will have my second surgery on my femoral artery do to the failure of the stents.
Regina Heller