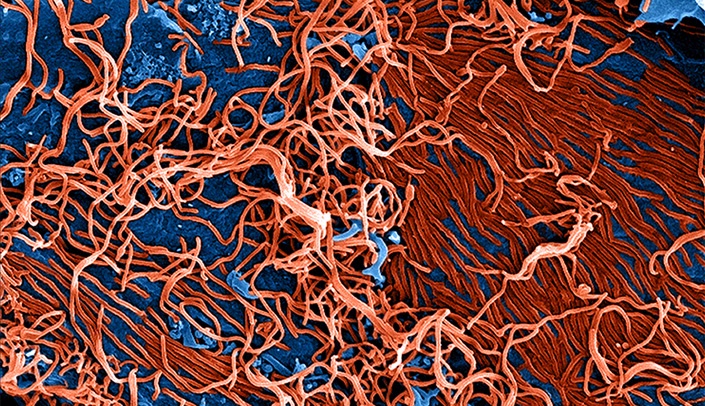
The 2014 Ebola outbreak has been one of the most devastating public health crises in recent history.
It’s an ever-evolving story that has stretched from West Africa to Omaha.
The virus, which presents like malaria or flu in its early stages, initially caught health care professionals by surprise as it spread through eight West African countries. At press time, the death toll had reached more than 8,600, including nearly 350 health care workers.
In the United States, fear of the virus spread more easily than the virus itself and led to anxiety, false alarms, airport screenings and forced quarantines.
Cooler heads prevailed in Nebraska, however, where three patients were sent for treatment in September, October and November.
Two men, who contracted the virus in Liberia, were successfully treated and released at UNMC. A third, who had been in Sierra Leone and arrived in extremely critical condition, died despite heroic efforts to save him.
Why UNMC? UNMC has had a long-term focus on many infections, including dangerous emerging infections like Ebola. UNMC already is home to world-class research in HIV-AIDS, malaria and methicillin-resistant Staphylococcus aureus (MRSA).
The Nebraska Public Health Laboratory was developed on the UNMC campus in 1997 to provide the biosafety level 3 (BSL-3) laboratory necessary to not only test but do research on many highly contagious and pathogenic organisms as smallpox, anthrax, tularemia, avian influenza, Lyme disease, West Nile virus and Ebola. (See story page 7.) In this facility, many infectious disease researchers are working on strategies for early diagnosis, vaccines, and other treatments for these diseases (See story page 8.)
The laboratory had been building and strengthening its expertise in emergency preparedness long before the 9/11 terrorist attacks on the United States. In 2005, UNMC developed the Nebraska Biocontainment Patient Care Unit as a collaborative project with the Nebraska Department of Health and Human Services and Nebraska Medicine to be prepared to care for individuals who have highly infectious diseases. The unit also has been proposed to the Department of Defense to be used to study new treatments for these diseases.
The largest of three biocontainment units that accept Ebola patients in the country, UNMC developed protocols that became the national standard for treatment thanks to the team’s experience in biopreparedness through quarterly drills conducted over many years. At times, Philip Smith, M.D., medical director of the Biocontainment Unit and professor of infectious diseases, felt pressed to justify the existence of the unit.
Each training drill, however, brought more refinements to the protocols – from personal protective equipment (PPE) and waste disposal to transportation and patient mental health.
With the arrival of Ebola patients, the protocols were implemented, but other opportunities and challenges arose.
There was a need to swiftly obtain and test new treatments. Chris Kratochvil, M.D., associate vice chancellor for research, worked collaboratively with Jon Beck, Pharm.D., nurse LuAnn Larson and Scott Koepsell, M.D., to obtain these treatments, sometimes from other countries.
They also had to develop protocols and obtain emergency permission to administer such drugs as ZMapp and TKM Ebola.
Partners in this process included UNMC’s Institutional Review Board, Emory University, the National Institutes of Health, the Food and Drug Administration and the White House.
Innovations in use of bedside diagnostics were developed by Steven Hinrichs, M.D., Stokes-Shackleford Professor of Pathology and Microbiology and department chairman; Pete Iwen, Ph.D., director of the Nebraska Public Health Laboratory (NPHL) and professor of pathology and microbiology at UNMC, and others.
Team members solved each of these issues with innovation and ingenuity.
UNMC’s innovations in transport, use of personal protective equipment, and waste disposal were not only extremely effective but caught the attention of the Centers for Disease Control and Prevention (CDC) and health organizations throughout the world. (See story below.)
Health teams have since turned to UNMC for best practices, which have become the gold standard in Ebola care, and UNMC has become one of two training sites for a larger number of designated hospitals helping the nation prepare to care for Ebola patients, if needed. (See story page 9.)
UNMC continues to work on new diagnostics, design of clinical trials that will be used in the U.S., as well as Africa, and how the genetics of the virus determines how it infects a person.
On another emergency preparedness front, UNMC researchers are helping to combat weapons of mass destruction as part of a collaboration between the University of Nebraska and the United States Strategic Command.
With the partnership, the University of Nebraska’s National Strategic Research Institute (NSRI), was established in the fall of 2012. The institute is one of 13 University-Affiliated Research Centers across the United States. NSRI focuses on five core research competencies in support of the United States Strategic Command, the Department of Defense and other agencies. (See story page 8.)
Recently, the World Health Organization asked UNMC to join its Global Outbreak Alert and Response Network (GOARN), a 300-plus worldwide network of institutions that react rapidly to outbreaks of international importance to cut response time to days and hours. These developments are part of a strategic plan designed to position UNMC and Nebraska Medicine as leaders in the field of biocontainment and emergency preparedness.