 |
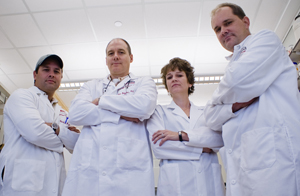
UNMC’s “Staph Team,” from left: Paul Dunman, Ph.D., Ken Bayles, Ph.D., Tammy Kielian, Ph.D., and Paul Fey, Ph.D. (Photo by Andrew E. Nelson, UNMC public relations) |
Team member Ken Bayles, Ph.D., professor of pathology/microbiology just received an $11.1 million program project grant from the National Institutes of Health (NIH). It is the largest research grant ever to be awarded to UNMC’s department of pathology/microbiology and is the only program project grant given by the NIH to investigate MRSA.
The team, a powerhouse of basic science and clinical experts who are focused on hospital-induced infections, aims to conquer CA-MRSA, which has become resistant to most standard antibiotics and is becoming more resistant to newer ones. Researchers have nicknamed it the “superbug.”
A strong project
Tom Rosenquist, Ph.D. vice chancellor for research, said only the most well-recognized, interactive, productive senior scientists are able to put together and manage the kind of large-scale projects that merit the multi-million dollars that come with a program project grant.
|
Grant to fund several projects
The five-year, multi-investigator/multi-institutional grant funds four projects, three from UNMC, that tap investigators from different, yet complimentary areas of expertise. The fourth project continues collaboration with an investigator at the University of Iowa.
“This is a prestigious grant and demonstrates that UNMC’s concentrated expertise is getting national attention,” said Paula Turpen, Ph.D., director of research resources.
The team has expertise in varied aspects of staph including biofilm development, gene regulation, physiology and the immunology of staph infections. The hypothesis to be tested is that staph biofilm formation involves complex developmental processes that affect the host immune response, Dr. Bayles said.
Team to examine how staph grows
The researchers seek to understand how staph bacteria grow in animals to cause disease — using a mouse model that has genetic variances to test various outcomes. They also will look at the mechanism behind biofilm development — how it forms and becomes resistant to the body’s natural immune response and to antibiotics.
Steven Hinrichs, M.D., professor and chairman of pathology/microbiology, said this is an important grant because it positions UNMC for the future.
“Ken and his team have made remarkable progress in a short time and I know even greater things are ahead,” he said.
Staph prevalence alarming
Staph, which is present on the skin or in the nose of healthy people, is the cause of some of the most common minor skin infections in the United States. It has historically been a leading cause of hospital infections in humans worldwide. In the past several decades, the emergence of MRSA, which is resistant to multiple antibiotics, has left relatively few therapeutic options available.
Staph causes 1.7 million infections and approximately 100,000 deaths each year in the United States. Surgical sites and the bloodstream are common targets, but it also causes pneumonia. Catheters, pacemakers and any implant device, such as hip and knee replacements, are prone to infection. Nosocomial bloodstream infections are a leading cause of death in the United States.
Drug resistance on the rise, too
Over the past decade, health care surveillance officials have seen a remarkable increase in resistance among community- and hospital-acquired pathogens that were routinely susceptible to such antibiotics as penicillin and methicillin and even vancomycin, the traditional drug of “last resort.”
Currently, about 50 to 60 percent of staph infections are resistant to multiple kinds of antibiotics. Not only are hospital-acquired MRSA infections on the rise, but so are MRSA infections in those living in the community.
Public health threat grows
Today, these strains now pose a serious public health threat, causing more deaths per year than HIV-AIDS.
“Now, healthy young people are getting staph infections and develop complications that, in some cases, can lead to death,” Dr. Bayles said. “It’s because this new strain of MRSA, which was first identified about four years ago, is not only resistant to methicillin but also has a lethal combination of virulent traits.
“Unfortunately, it’s not clear why this strain is so deadly.”