 |
Research tools used by Yuri Persidsky, M.D., Ph.D., and Raghava Potula, Ph.D., include the digital imaging system for analyzes of brain tissue and cells affected in HIV-1 dementia. Dr. Persidsky, is senior author of a research article recently published in the prestigious journal Blood. Dr. Potula, a post-doctoral research associate, is first author of the paper. |
HIV-1 causes acquired immunodeficiency syndrome (AIDS). People with AIDS are at an increased risk for developing certain cancers and for infections that usually occur only in individuals with a weak immune system. The hope is to ultimately design a new, more potent treatment for AIDS patients, as well as have more broad applications in cancer and other immune disorders treatment.
The findings are published in the Oct. 1 issue of Blood, a prestigious journal of the American Society of Hematology. In addition to the research paper, the issue will feature and editorial comment on the importance of this finding. The enzyme is Indoleamine 2,3-dioxygenase (IDO).
“Our hypothesis is that IDO inhibition may offer the immune system a better way to fight off production of the virus,” said Yuri Persidsky, M.D., Ph.D., associate professor, UNMC Department of Pathology/Microbiology, and Pharmacology and Experimental Neuroscience.
“We think when cells of the immune system are infected with HIV-1, they produce toxins in the brain cells. This impairs brain cell function, and leads to HIV-associated dementia,” said Dr. Persidsky, senior author of the paper. “By suppressing IDO, we were able to see a decrease in the amount of HIV-1 in the brain. This is significant because it’s difficult to control virus in the brain.”
The study is the first to demonstrate beneficial effects of IDO suppression to improve immunity against HIV-1 infection.
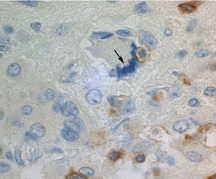 |
A microphotograph acquired by an imaging system demonstrates an HIV-1 infected cell being attached (see black arrow) and destroyed by a CD8 lymphocyte (brown stain) in the brain of experimental animal. The similar process occurs in human HIV-1 brain infection. Researchers found that IDO inhibition increased elimination of virus-infected cells in mouse models. |
The immune system protects organisms from infectious agents like bacteria, parasites, viruses, rapidly growing cancer cells, and other noxious agents. Specific markers — called antigens — on the surface of these invaders are recognized as foreign to the body, which allows cells of the immune system to attack and destroy them.
“IDO-enhanced expression and activity diminishes the intensity of responses against antigens recognized as alien,” Dr. Persidsky said. “It appears to regulate the magnitude of such immune responses.”
He said research has suggested that high levels of IDO activity in infected individuals contribute to a poor efficiency of immune responses against the virus-infected cells. This permits tumor cells or noxious agents (bacteria and viruses) to escape destruction and replicate in uncontrolled fashion, leading to tumor development and serious life-threatening or chronic infections, like HIV-1.
The research team studied the effect of IDO in a mouse model developed by Dr. Persidsky and UNMC researchers Larisa Poluektova, M.D., and Howard Gendelman, M.D. The model reproduces features of HIV-1 infection in the brain, internal organs and blood, and was able to demonstrate that specific anti-viral responses are significantly enhanced in animals treated with an IDO inhibitor.
David Munn, M.D., co-author of the paper, said it is not known what the clinical significance of the IDO mechanism might be in human HIV-1 infection. “However, there is an intriguing link between the expression of IDO in HIV infection and the expression of IDO in patients with cancer,” said Dr. Munn, professor of pediatric oncology, Medical College of Georgia.
“If the HIV-1 virus uses IDO to create a similar immunosuppressive effect, which is still just at the stage of speculation, then this could open the possibility of adding anti-IDO drugs (IDO inhibitors) as an additional treatment for patients with HIV infection,” said Dr. Munn. He and others hypothesize that IDO may act in cancer patients to help tumors escape the patient’s immune system.
UNMC psychiatrist, Carl Greiner, M.D., sees many patients with AIDS. “Losing mental capacity is one of the most frightening prospects of AIDS,” he said. “Research work to improve our understanding of treatment of AIDS dementia is a top priority.”
UNMC AIDS physician Susan Swindells, M.D., said the potential for Dr. Persidsky’s research is important. “We know that the immune system can control the virus to a degree, but this is not enough,” Dr. Swindells said. “Dr. Persidsky and his group are exploring an entirely new area of potential therapy, by manipulating the immune system to help it control the virus better.
“This is a very creative approach and also illustrates the value of their mouse model, which was developed here at UNMC,” she said.