 |
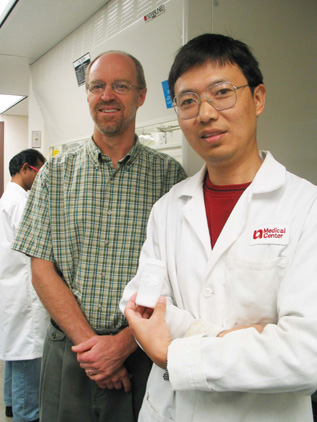
Yuxiang Dong, Ph.D., research associate, UNMC College of Pharmacy, far right, holds a bottle of the compound developed into what he and Jonathan Vennerstrom, Ph.D., associate professor of pharmaceutical sciences, UNMC College of Pharmacy, center, hope will be the next and best anti-malarial drug on the market. Working in the background is researcher Kamaraj Sriraghavan, Ph.D. |
In the article, lead author Jonathan Vennerstrom, Ph.D., associate professor of pharmaceutical sciences, UNMC College of Pharmacy, describes the development of an anti-malarial drug candidate, which has been lauded by the World Health Organization (WHO).
The team, made up of scientists from the UNMC College of Pharmacy, Monash University in Australia, the Swiss Tropical Institute and the F. Hoffmann-LaRoche pharmaceutical company, has received $5.5 million in funding from Medicines for Malaria Venture (MMV) of Geneva, Switzerland.
Dr. Vennerstrom said the anti-malarial drug candidate is undergoing phase I clinical trials in London, where Ranbaxy Laboratories Ltd., MMV’s pharmaceutical partner, has obtained authorization from Medicines and Healthcare Products Regulatory Agency to conduct clinical trials in the United Kingdom. The trials will evaluate the safety of the drug candidate in a small group of healthy human volunteers. This is the first regulatory step in new drug development after efficacy and safety is established in the pre-clinical phase.
If successful, the drug candidate could become a major new weapon against multi-drug resistant malaria.
“The need to develop a low-cost, potent synthetic antimalarial drug is more urgent than ever,” said Christopher Hentschel, Ph.D., chief executive officer, MMV. “We are very excited about this project; it has surpassed our expectations as it moved so successfully and rapidly through candidate selection.
“The publication of its development in Nature is another validation that the team has done a fantastic job in moving the project forward with professionalism, dedication and speed. This could be the biggest breakthrough in malaria treatment in 80 years,” he said.
“The article is very exciting and may represent the most important new discovery since the Chinese isolated Artemisinin and used it to treat malaria,” said J. Carl Craft, M.D., chief scientific officer, Medicines for Malaria Venture. “The synthetic peroxides appear to have the potential of increased activity and at a lower cost when compared to artesunate. We hope that it become a treatment used to treat malaria.”
The new drug candidate is the first to be entirely funded by MMV, Dr. Vennerstrom said.
“We were pretty amazed about getting published in Nature,” Dr. Vennerstrom said. “I’ve been blessed with all the people in the lab and our partners.”
Yuxiang Dong, Ph.D., research associate, UNMC College of Pharmacy, said when he discovered the compound of the drug candidate years ago, he never expected it to progress this far. Called the Synthetic Peroxide Project, in 2001 it was voted Project of the Year by MMV.
MMV was officially launched in 1999 as a non-profit foundation dedicated to reducing the burden of malaria in disease endemic countries by discovering new affordable anti-malarials through effective public-private partnership.
“Ranbaxy is privileged to carry on the baton from this team of talented researchers. Our scientists are excited to be able to work on a drug that could save millions of lives,” said Brian Tempest, Ph.D., chief executive, Ranbaxy Laboratories.
“We are pleased with the progress of the project. Developing drugs is not easy. We have many hurdles to overcome, but we will rise to the challenge. We are committed to developing a drug that is not only safe and effective, but also affordable to people in India and hundreds of millions of others who have to live with this terrible disease every day.”
The resurgence of malaria, starting in the late 1970s, is largely attributable to drug resistance, according to MMV. The standard cheap medicines, such as chloroquine, are rendered useless in almost every corner of sub-Saharan Africa, where every 30 seconds a child dies of malaria. More than 1 million people die each year from this curable disease.
The most effective antimalarial now is ACT (artemisinin-based combination therapy). Because of its cost, donors have been reluctant to provide the necessary subsidies to make ACT accessible for the 300 million to 500 million treatments which are needed every year.
Malaria kills more than 2 million people each year in places such as Africa, Asia, Central and South America, according to WHO. In addition, an estimated 300 million to 500 million new cases of malaria are diagnosed each year. More than 90 percent of all malaria cases occur in Africa. Also at risk are those who travel to countries where malaria is prevalent.
Other authors on the paper are: Sarah Arbe-Barnes, Fulcrum Pharma Developments Ltd, United Kingdom; Reto Brun, Swiss Tropical Institute, Basel, Switzerland; Susan A. Charman, Victorian College of Pharmacy, Monash University, Australia; Francis C. K. Chiu, Victorian College of Pharmacy; Jacques Chollet, Swiss Tropical Institute; Yuxiang Dong, Ph.D., UNMC; Arnulf Dorn, Daniel Hunziker and Hugues Matile, F. Hoffmann-La Roche Ltd.; Kylie McIntosh, Victorian College of Pharmacy; Maniyan Padmanilayam, UNMC; Josefina Santo Tomas, Christian Scheurer, and Bernard Scorneaux, Swiss Tropical Institute; Yuanqing Tang, UNMC; Heinrich Urwyler, Basilea Pharmaceutica Ltd., Basel, Switzerland; Sergio Wittlin, Swiss Tropical Institute; and William N. Charman, Victorian College of Pharmacy.