The victims are varied, from thousands of sea lions off the coast of Peru to mink farmed for fur in Spain to grizzly bears in Montana and harbor seals in Maine. For months, the avian influenza virus that has been decimating birds across the world has also sickened and killed a menagerie of mammals, raising fears it might evolve to spread more efficiently between these animals, and ultimately between people.
For that nightmare to unfold, however, the virus, a subtype known as H5N1, would have to undergo a major transformation, changing from a pathogen efficient at infecting cells in the guts of birds and spreading through feces-contaminated water into one adept at infecting human lung tissue and spreading through the air. So far, that has not happened. None of the few people who have caught the virus currently wiping out birds, called clade 2.3.4.4b, seems to have passed it on to other people.
“This clade … is most of all and more than all previous clades an avian virus,” says virologist Martin Beer of the Friedrich Loeffler Institute. That is why it has spread so far and wide in birds, he says, and why it is so poor at infecting people. Beer and his colleagues in Berlin and Münster, Germany, have been using lung tissue taken from cancer patients undergoing surgeries, for instance, to see whether the virus can efficiently infect the human cells. So far, it cannot.
So exactly how would this virus have to mutate to cause a human pandemic? Scientists can’t fully answer that yet—but they have identified some key steps. Much of what is known comes from controversial experiments more than a decade ago in which researchers coaxed an earlier strain of H5N1 to spread more efficiently between ferrets. That feat prompted restrictions on such “gain of function” experiments, which has hampered research, says Mathilde Richard, a virologist at Erasmus Medical Center, where some of that work was done. “I do think that this has really, really slowed down our knowledge.” Still, researchers have found other ways to examine how avian flu adapts to mammals. For instance, when another avian flu subtype called H10N7 struck seals in Europe in 2014, scientists sequenced the virus at different stages of the outbreak to identify what genetic changes helped it adapt to the mammals. “That is sort of like a massive gain-of-function experiment in nature, and from those outbreaks, you can still learn quite a lot,” Richard says.
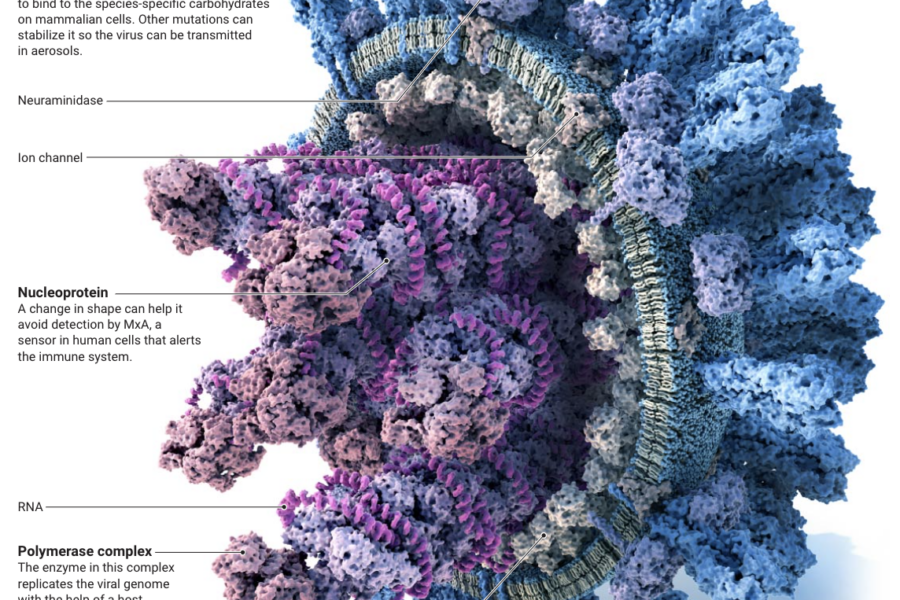
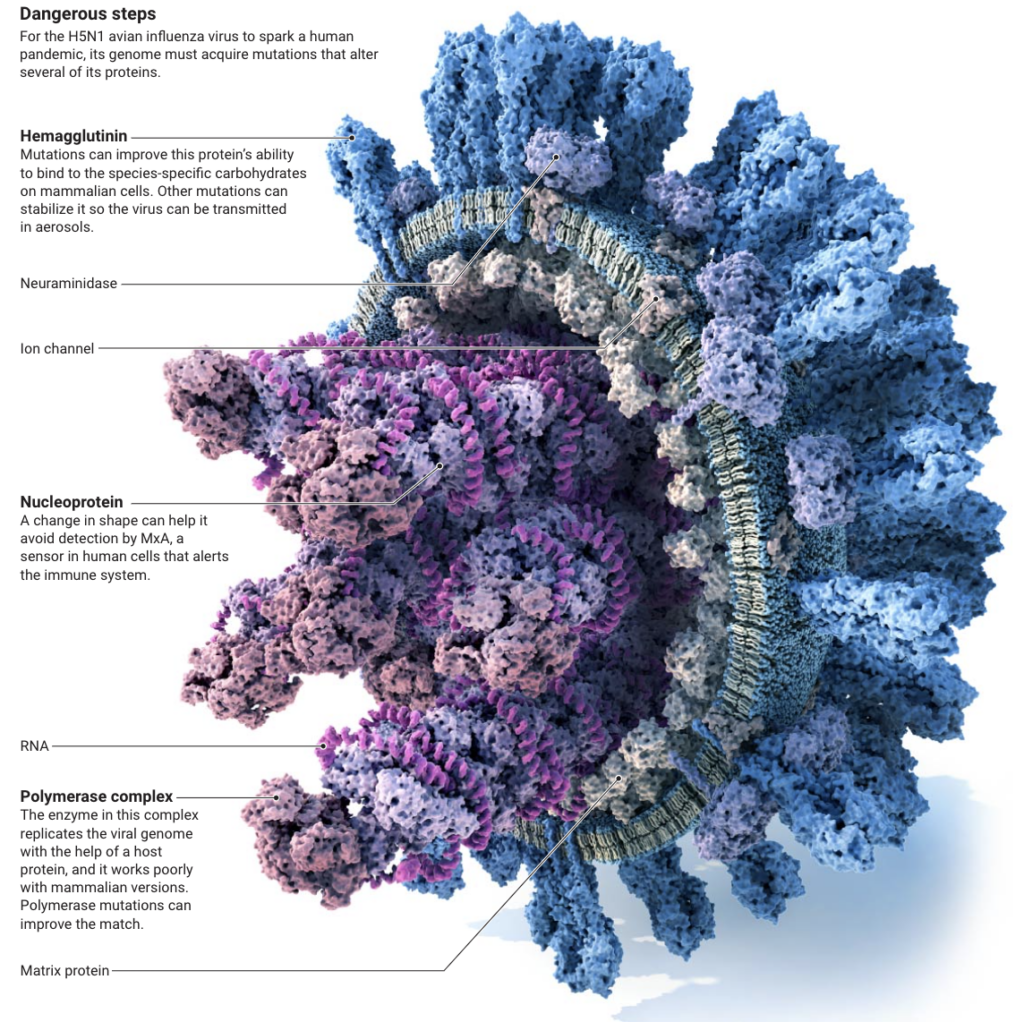
Virologists now know that for H5N1 to become adept at spreading between mammals, several of its proteins must evolve. One they are watching closely is the polymerase the virus uses to replicate its RNA genome once it invades a cell. To do its job, the enzyme must co-opt a host intracellular protein, and it is currently more tailored to the avian molecule than its mammalian equivalent. Different combinations of mutations in one subunit of the polymerase, PB2, can change the enzyme to work better in mammals. But there’s one known mutation, dubbed E627K, that does so in a single bound by swapping an amino acid at a key position, a glutamate, for a lysine. The mutation’s first recorded appearance was in the virus causing the 1918 flu. “That PB2 was so good that it has stuck in every human influenza virus until the 2009 swine flu pandemic,” says Imperial College London virologist Tom Peacock.
Whatever path the virus hits upon, H5N1 needs an altered PB2 to become a human pathogen. Think of evolving into a pandemic virus as a ladder that H5N1 has to climb, Beer says. “Then this is the first step.”
It seems an easy step. H5N1 has managed it several times already in the current avian flu virus outbreak. For instance, researchers found the E627K mutation in infected foxes that were sampled in the Netherlands in late 2021 and early 2022. The mutation was also found in a sample from a New England seal, part of an outbreak of H5N1 in seals off the East Coast last year. The PB2 mutations don’t seem to hamper the virus in birds, Richard says. “That’s the reason why we see the polymerase mutations popping up quite often.”
But for H5N1 to cause a pandemic it also needs multiple changes in hemagglutinin, a protein on the surface of the virus that helps it attach to carbohydrates on host cells. Those carbohydrates are shaped differently in birds and mammals, so H5N1’s hemagglutinin has to change its shape for the virus to efficiently infect mammalian cells. “That is absolutely essential,” Peacock says. “In fact, there are no influenza viruses that are transmissible between people that don’t have a human-adapted hemagglutinin.”
A pair of amino acid changes, Q226L and G228S, can reshape hemagglutinin to bind to mammalian cells. But in H5N1, the second amino acid change requires two nucleotide mutations very near each other in the hemagglutinin gene. “That is much rarer than single nucleotide changes,” Peacock says. “But obviously, if you put it under enough selection pressure, it could maybe do that.”
Another crucial hemagglutinin change would make H5N1 more transmissible through the air—also a prerequisite for a pandemic. Once the virus attaches to a cell it is taken up into a vesicle that becomes more acidic, triggering a pH-dependent shape change in the hemagglutinin. This leads the virus and vesicle membranes to fuse, letting the pathogen’s genetic material escape into the cell. In water, the hemagglutinin on avian viruses typically has no problem staying untriggered. But in the air, droplets of moisture carrying flu viruses often shrink and may reach that acidic threshold, so pandemic viruses need mutations that stabilize their hemagglutinin, explains Emory University virologist Seema Lakdawala, who studies airborne transmission of pathogens.
Those three steps are the minimum changes H5N1 likely needs to become transmissible between humans, Richard says. In her lab she regularly sequences H5N1 viruses isolated from mammals to see whether they carry any of these concerning mutations. Her team also directly tests the virus’ polymerase activity and the binding capacity and stability of their hemagglutinin. “We really want to test the phenotypes and not just look at the genetic changes because we know that there are probably [other genetic changes] that have the same impact and we just do not know them yet.”
Beer thinks a pandemic virus needs a fourth change: an ability to evade an intracellular protein called MxA. MxA alerts the immune system to an influenza infection when it detects the virus’ nucleoprotein, a protein bound to its RNA. To prevent that alarm, the nucleoprotein must mutate into a form that the human MxA cannot detect. “That is the last barrier,” Beer says. Although MxA’s detection skills appear very weak in ferrets and some other animals, it is more sensitive in humans—and in pigs. “If an H5 virus is spreading in pigs then it really is code red,” Beer says.
In an unpublished experiment Beer and his colleagues infected pigs with H5N1. Even when high doses were used, the virus barely replicated in the animals. People likely have other defenses beyond MxA that avian flu viruses have to beat. For instance, in a recent preprint researchers found that another protein in humans called BTN3A3 also detects the nucleoprotein of avian influenza. And Lakdawala thinks that even though most people have not been exposed to H5 viruses, life-long exposure to other flu viruses may have created cellular or antibody protections against H5N1, too. In an ongoing experiment she is comparing how the current avian virus grows in ferrets infected 3 months earlier with seasonal influenza versus ferrets with no prior infections. “We really want to understand how likely these viruses are to emerge in the context of pre-existing immunity,” she says.
What researchers know so far about the steps needed to adapt H5N1 to humans offers some reassurance: It has one of the highest barriers to becoming a pandemic virus of any avian influenza virus, Peacock says. “It’s really wrong in so many ways,” he says. “But obviously it only has to get the right combination of mutations once to do to jump.”
And with the virus spreading so furiously around the globe, it has more opportunities to hit the right combination than ever before. In the past, H5N1 outbreaks have faded, but this time, the virus is probably here to stay in wild birds in Europe and the Americas, Richard says. “This is the threat that’s going to keep knocking at our door until it will indeed, I assume, cause a pandemic. Because there is no way back.”